The history of anti-rheumatic medicines is one of hope and disaster
For decades, a lack of safe and efficient treatment meant that rheumatologists and their patients were caught between a devastating disease and harmful medicines. A new PhD investigates the history of the treatment of rheumatic diseases.
In the early years of rheumatology, rheumatoid arthritis ate away at joints of a large group of patients, and rheumatologists were banished to stand by and watch. In 1949, when treatment with cortisone – or with corticosteroids – was introduced, the nightmare seemed at last to have ended.
It seemed that science had produced yet another miracle cure, just a few years after penicillin had made its entry into medicine.
As if that was not enough: This time it was the body’s own resources – the hormones – that medical science had harnessed and put to work to strengthen the life processes of the human body.
A miracle cure?
When science journalist John E. Pfeiffer described the breakthrough in Popular Science in the summer of 1951, he wrote:

“The hormones [ACTH and cortisone] represent an entirely new approach in the art of healing. Penicillin, streptomycin, the sulfa drugs, and most other medicines you’ve been reading about are poisons intended specifically to attack invading germs. (…) But ACTH and cortisone are not germ-killers. They are natural products, gland hormones. They influence the body’s built-in chemical factories that go into action whenever extra supplies of tissue are required.”
For a while, it seemed as though nearly any disease could be treated with steroid hormones – and in the treatment of nearly any disease the new drug was attempted—often with remarkable effect.
In the treatment of rheumatoid arthritis, the effect was spectacular.
For the first time, it seemed as though rheumatologists were not merely able to sooth their patients’ pain, but to actually stop their disease.
Pfeiffer, in his enthusiasm, went even further:

“The hormone can reshape (…) a deformed joint into a smoothly working fulcrum. Pain disappears, and the accumulated debris dissolves. Furthermore, destruction of supporting tissue is stopped in its tracks for months and fresh cells may come in to repair the damage.”
Read More: Drugs that didn’t keep their promise
A prize won and a price paid
Science had once again emerged victorious. Euphoria was sweeping across the world of medicine. The men who had come up with the idea had been awarded the Nobel Prize in Physiology and Medicine already the previous year. In the decade that followed, thousands upon thousands were to be treated with cortisone.
Soon, however, health professionals began to observe a number of side effects in their patients – such as skin damage, small wounds, osteoporosis, diabetes; and impaired immune defense. It even turned out that cortisone reduced the capacity of the body to repair certain damages.
The side effects seemed to strike nearly anywhere – and they were severe, devastating. Some patients had their skin destroyed by cortisone, others their bones.
Gradually, the relationship between the drugs and the damages was established. Cortisone treatments had to be discontinued and patients once again found themselves in a situation where their disease broke down one joint after another, with no existing drug to stop it. On top of that, some patients had now had their skin destroyed; in others the cortisone treatment had harmed the bones.
Their suffering was gradually forgotten
Most likely, no-one recorded the histories of the tens of thousands of patients who in the course of the 1950s got their already vulnerable existences turned upside-down by cortisone treatment. Adverse events are not the kind of events from which one build the grand History of Medicine. Most probably, no-one systematically recorded these patients’ stories or collected their files to write down their history.
In many of these cases, as in all cases of adverse events, it must have been difficult even to establish that the observed damages were drug related. Most probably, a lot of patients never got to know that it was their medicine that had hurt them.
Perhaps it was better that way.
Perhaps it salvaged their trust in the health workers on whom they depended for their continuing treatment. The patients whom the cortisone and the disease had hurt the most, had other worries and concerns to tend to. As had their families.
And rheumatology turned its attention towards the future, allowed the past to be the past, and looked for new solutions.
Read more: Promising remedy for rheumatism
The “second victims” of maltreatment
Based on what we today know about cortisone and about the extent to which it was used during the 1950s, we can but attempt to imagine how this trajectory – through euphoria and despair, through hope, relapse and desillusion – may have been for the individual patient.
For rheumatologists, the crisis must also have been a profound one.
The drug they had hoped would be the wonder drug they had lacked turned out to be the almost exact opposite. That was a set-back for the professional community.
For thousands of individual physicians it must have been fundamentally tragic to experience that their arthritic patients had their bodies destroyed by the drugs they had prescribed exactly in order to prevent destruction.
Physicians may themselves have been traumatized. They may have become what more recent professional jargon have termed ”second victims”.
Reassurance in “non-steroidal” drugs (NSAIDs)
By the end of the 1950s, cortisone had thus been over-used and prescribed for all sorts of conditions, and caused enormous damage.
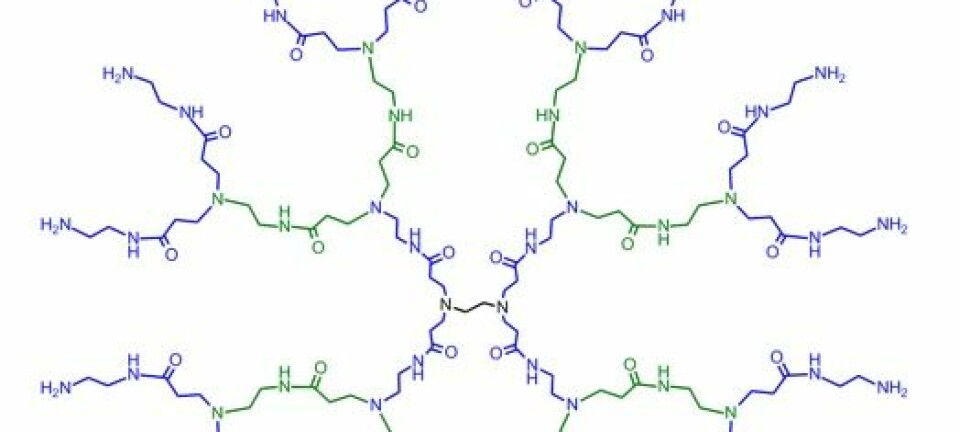
Two young scientists, Michael W. Whitehouse and James W. Lash, were at the time working at the University of Pennsylvania, the one a floor above the other, and as they were introduced to each other, they devised an experiment that would allow them to study how different anti-inflammatory compounds slowed down the development of cartilage in chicken fetuses.
In addition to testing the impact of the steroid hormones cortisone and hydrocortisone, and of their synthetic analogues, they also tested the effect of potassium salicylate, potassium benzoate, potassium thiosalicylate, phenylbutazone, and cincophene.
It was not obvious what characteristics the latter substances shared beyond their anti-inflammatory application -- and the fact that they were not steroids. When Whitehouse organized the text that described the results from their experiments, he therefore separated between steroids and non-steroids.
Read More: Synthetic supermolecule to fight cancer, arthritis and herpes
The term “non-steroid” was thus born – from serendipity.
For Whitehouse did not aim at introducing a new drug category. He simply needed to draw a line between those substances that were steroids, and the others. And yet, the expression that he thus carved out offered to draw a boundary that a lot of other actors, in a lot of different contexts, also needed to draw.
Researchers, physicians, bureaucrats, and others could hence present new preparations as non-steroidal, and neither they nor their clients or patients needed concern themselves with fears for side effects of the kind the cortisone preparations were now known to cause.
Within a few years, Whitehouse’ pragmatic formula “non-steroid” became a fixed expression. Soon the expression “non-steroidal anti-inflammatory drug” gained the kind of currency that would allow its acronym “NSAID” to become a word on its own. Gradually it became difficult even to imagine a conversation about arthritis or rheumatology without these five letters.
A trojan pill course: NSAID also had side effects
Yet, during the 1980s and 1990s, evidence accumulated that also NSAIDs – the supposedly safe alternative to steroids – had their own severe side effects.
Gradually, professionals became aware of the emerging patterns: Pregnant women miscarried or gave birth to premature children a little more often after having taken NSAIDs to sooth their pain. In others, the kidneys failed in peculiar ways.
It was however the gastrointestinal damages that caused the most worries – and the highest numbers of deaths.
The NSAIDs could in in fact attack the stomach at two fronts at once: They were acids, and thus already tough for the stomach. However, when these drugs reached the digestive organs via the blood stream, they could, like a Trojan horse, turn off the digestive organs’ anti-acid defenses. All of a sudden an ulcer would appear. At worst, a bleeding one. At the very worst, a deadly one.
Read More: What are the major challenges to modern medicine?
Progress and new optimism
Hence, there was a surge of optimism when several pharmaceutical companies, towards the end of the 1990s, announced that they had developed a new kind of NSAIDs – namely the selective COX-2 inhibitors – and that these did not put the same strain on stomach and bowels.
In 1999, Pfizer launched Celebrex (celecoxib). Later the same year, the competitor launched its alternative, Vioxx (rofecoxib), in what was the company’s “biggest, fastest and best launch ever”.
It was a breakthrough that physicians and patients had been waiting for. A riddle seemed to have been solved, and the new NSAIDs were a great success, also commercially.
But then it emerged, in what was plausibly that decade’s greatest pharmaceutical scandal, that the new kind of NSAIDs significantly increased risk for heart disease and death.
In 2004, Vioxx was withdrawn from the marked. During the five years Vioxx was in use, the FDA later estimated that the drug alone had caused tens of thousands of deaths only in the USA.
Behind every number was a person in pain
It requires a bit of fantasy and a tad of effort to imagine that behind each and every one of those deaths there has been a person – a person who has sought relief from pain. Some of these had probably fought their rheumatic diseases for decades already – first with cortisone, then with NSAIDs. They had perhaps had both their skin and their intestines ruined – before Vioxx or Celebrex emerged as their salvation.
Then one day the blood clot struck.
Others were perhaps women whose skin had turned to rice paper after years of cortisone treatment, who at last saw their red, swollen joints find peace. Before one sudden day they sensed something clearly unpleasant and yet unmistakably undefinable deep down in their throat – as though they had swallowed too much macaroni in one go – without knowing that that’s what heart infarctions may feel like for women.
These rheumatic patients did perhaps not even call for help. They were too accustomed to endure pain and unpleasant feelings even to consider it.
Towards the 1980s, cortisone was gradually reintroduced in the treatment of rheumatic diseases – albeit in smaller dosages, with lower ambitions, and with more caution. And while cortisone treatment was reaccepted in the mainstream, the NSAIDs thus developed their own problematic profile. The time when it sufficed to state that a drug was not cortisone in order to have it accepted as safe, was gone.
Read More: Human organs-on-chips may one day replace animal testing
A plea for curiosity
Ibuprofen is our kindest NSAID. Passing as Addaprin, Advil, Motrin and IBU among friends, it is for many as natural a part of our lives as the daily cup of coffee. The same goes for a series of over-the-counter cortisone preparations.
While commercials for all sorts of drugs now roll across our TV screens, the choice is uniquely ours when it comes to over-the-counter drugs. Our doctors will not meddle.
So we can let ourselves be seduced.
Yet, at the same time, we may also chose to dig into an encyclopedia as we settle in in front of our TV. We may access MedlinePlus, Drugs.com, and other pre-approved patient education web sites. We may cross-read with Wikipedia. And we may bring the fragments that we can remember from this text, and try to place the advertised medicines in a larger, more exciting context:
Is it a steroid medicine? Is it a non-steroid?
Not in order to find villains and heroes, but in order to map the genealogies of our drugs, and snoop in their family secrets.
How close family are Vioxx and that new pain ointment? Is that blue carbon tablet somewhat similar to the medicines that our old aunty Kitty was taking?
It may well be.
---------------
Read the Danish version of this article on Videnskab.dk
Buer successfully defended the PhD thesis “Rheumatologies in the making – An ethnography of meaning and interaction in a Norwegian hospital ward” on May 30 2017. The present text is inspired by his research paper “Origins and impact of the term ‘NSAID’” (Buer 2014). An earlier version was published in Norwegian in the Norwegian newspaper Aftenposten. He has more recently published research on the category of disease-modifying drugs: “A history of the term DMARD” (Buer 2015), and “To stop the erosion of hope: The DMARD category and the place of semantics in modern rheumatology” (Buer 2017).