ME/CFS may be linked to failure in energy supply to the cells
Researchers compared blood samples from patients with ME/CFS with those of a control group.
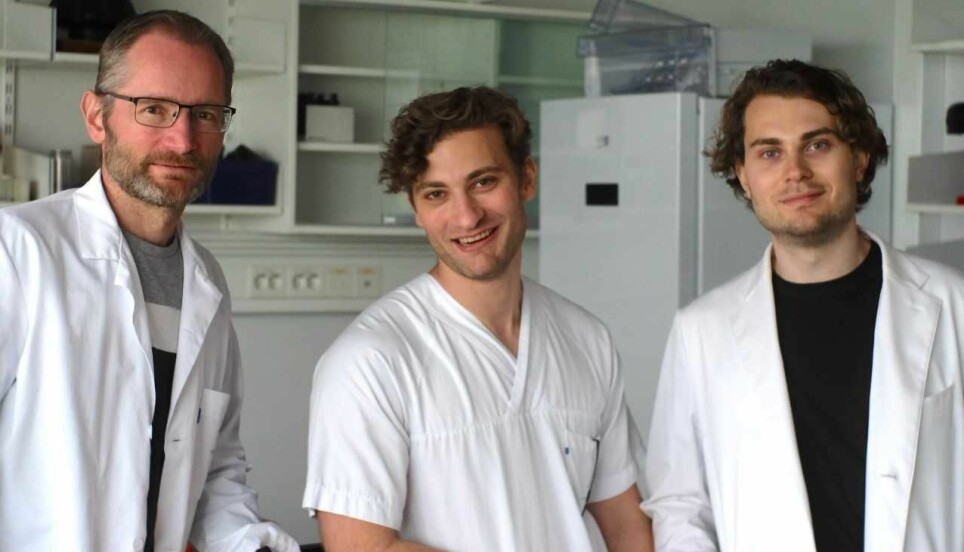
Researchers at the University of Bergen and Haukeland University Hospital were part of a research team for a new study that found differences in blood samples between ME/CFS patients and healthy people.
Patients with myalgic encephalomyelitis/chronic fatigue syndrome, or ME/CFS, had different levels of some substances that affect energy metabolism in the cells.
The cause of ME/CFS is still unknown. The main symptom is becoming abnormally exhausted from daily chores. Rest does not help as it usually would.
Other symptoms can include muscle aches, flu-like symptoms and hypersensitivity to light or noise.
The researchers believe the new findings could indicate that the cells of ME/CFS patients are struggling to obtain enough energy.
“What we think might be an explanation is that restricted blood flow during activity means the cells are receiving too little oxygen, and this leaves metabolic traces over time,” says Karl Johan Tronstad.
Tronstad is a professor in the Department of Biomedicine at the University of Bergen and has led the new study.
Measured 1700 substances in the blood
Metabolism involves vital chemical reactions that take place in the cells. The cells convert nutrients into energy, build new molecules and get rid of waste.
In the new study, the researchers performed an analysis of metabolites and other substances in blood samples from ME/CFS patients. Metabolites are metabolic products that are created when the cells convert different substances in the body.
The researchers analysed blood samples from 83 individuals with ME/CFS and 35 healthy controls.
The researchers measured about 1700 substances in the blood samples they took.
In the ME/CFS patients, they found an altered level of over 300 substances. Many of them involved the conversion of amino acids, which build up proteins, and lipids (fats).
“When you find such extensive changes in the pattern of amino acids and lipids, it indicates that something is going on with the energy metabolism,” says Tronstad.
Found common features
Not all the differences were shared by ME/CFS patients.
“There was a pretty large spread in the ME/CFS group’s data,” says Tronstad.
However, the ME/CFS patients had some of the changes in common as well.
Sixty-seven metabolic products clearly showed higher or lower levels in the ME/CFS group than in the controls. Overall, this suggests that amino acids and fats were used in a different way as fuel for the cells, according to the study.
“The results show what happens at the overall level in the body, and can indirectly tell us about conditions concerning the cells' energy metabolism,” says Fredrik Hoel, who also participated in the study.
“We’re talking about a metabolic shift towards utilizing other sources of energy than carbohydrates, such as fats and amino acids, which is something you observe in conditions where the body adapts to metabolic exertion,” says Hoel, who is a doctoral fellow at the University of Bergen.
Backup solutions
The researchers also measured hormones. Here they saw indications of energetic strain in the cells, according to Tronstad.
The researchers' hypothesis is that the cells are struggling to get enough energy, and that the metabolic changes are an indicator of this.
The cells initiate backup solutions to obtain enough fuel.
These changes are usually triggered when fasting, during strenuous physical activity or illness.
“We believe it’s an underlying failure in the energy supply that causes metabolic adjustments. Different systems are activated to keep energy production going continuously,” says Tronstad.
Subgroups with different patterns
The compensatory mechanisms are not necessarily the same from person to person.
The researchers found three subgroups among ME/CFS patients who had similar metabolic change patterns. In one subgroup, the patterns were associated with more severe symptoms.
“If one part of the system fails, you can initiate a reserve programme to save the situation. We think these reserves might be more individual, which could explain the different subgroups we’ve seen here,” says Tronstad.
August Hoel is a doctoral fellow and also participated in the study. He states that previous studies using the same methodology have been smaller.
“Statistically speaking, the patient group has a lot of variation, which has made interpreting similar types of studies challenging. Our advanced data analyses provide strong indications that the metabolic variation can be explained by metabolic subgroups with their own characteristics, but also with common features,” he says.
“Our study provides the most comprehensive overview of the metabolism of ME/CFS patients to date, which can help us and other researchers in further studies.”
Not just due to less physical activity
Tronstad addresses the question as to whether the differences between the ME/CFS groups and the control group are due to the disease or possibly to reduced activity levels.
“The overall metabolic changes weren’t related to the patients' level of function. However, one of the metabolic subgroups showed a link to poorer functional levels. This could mean that the metabolic consequences of a lack of physical activity over a long period of time are a negative factor, but this plays no decisive role in the disease mechanism itself,” he says.
The researchers hope the new findings from this study can be used for a more targeted search of new biomarkers and to simplify diagnosis.
Could an autoimmune mechanism lurk behind the condition?
Tronstad and his colleagues have long worked on the basis of a hypothesis that a failure of the immune system might be central to ME/CFS. The new findings could tell us something about the ripple effects of such a causal mechanism, according to Tronstad.
A few weeks ago, researchers Tronstad, Øystein Fluge and Olav Mella published another article in the Journal of Clinical Investigation in which they describe the hypothesis in more detail.
They suggest that the cause may be a disorder of the immune system that occurs after an infectious disease, for example. It is known that some people get ME/CFS after having mononucleosis.
The idea is that an autoimmune mechanism may be behind the condition. Autoimmunity is when the immune system attacks the body's own tissues.
“We think that the autoimmune mechanism might affect what’s called autoregulation of tissue blood flow,” says Tronstad.
“When we do an activity, the muscles have to adjust the blood flow to get enough. A higher work requirement requires more blood, causing the blood flow to be adjusted. If that adjustment doesn’t work well enough, the supply of oxygen and nutrients to the cells may be restricted.
Then the cells might need to adapt their metabolism, which may be the reason for the changes the researchers saw in the new study.
Research must continue
The proposal is a hypothesis – a working theory based on the knowledge that is available. The researchers need to test it further to find out whether it is correct or not.
“Finding autoantibodies and trying to figure out what kind of structures they bind to and so on is a really difficult task. Researchers of several other diseases are also struggling to figure this out. But we have some evidence that this could be an important factor in ME/CFS,” says Tronstad.
The new study and other similar studies in the ME/CFS field share some commonalities,” says Fredrik Hoel.
“There are also several ME/CFS studies that point towards the possibility of disturbances in regulating blood vessel function. This gives us a basis for forming a hypothesis that the metabolic changes are adaptations that might be due to the cells not receiving an optimal supply of oxygen,” he says.
Thorough study
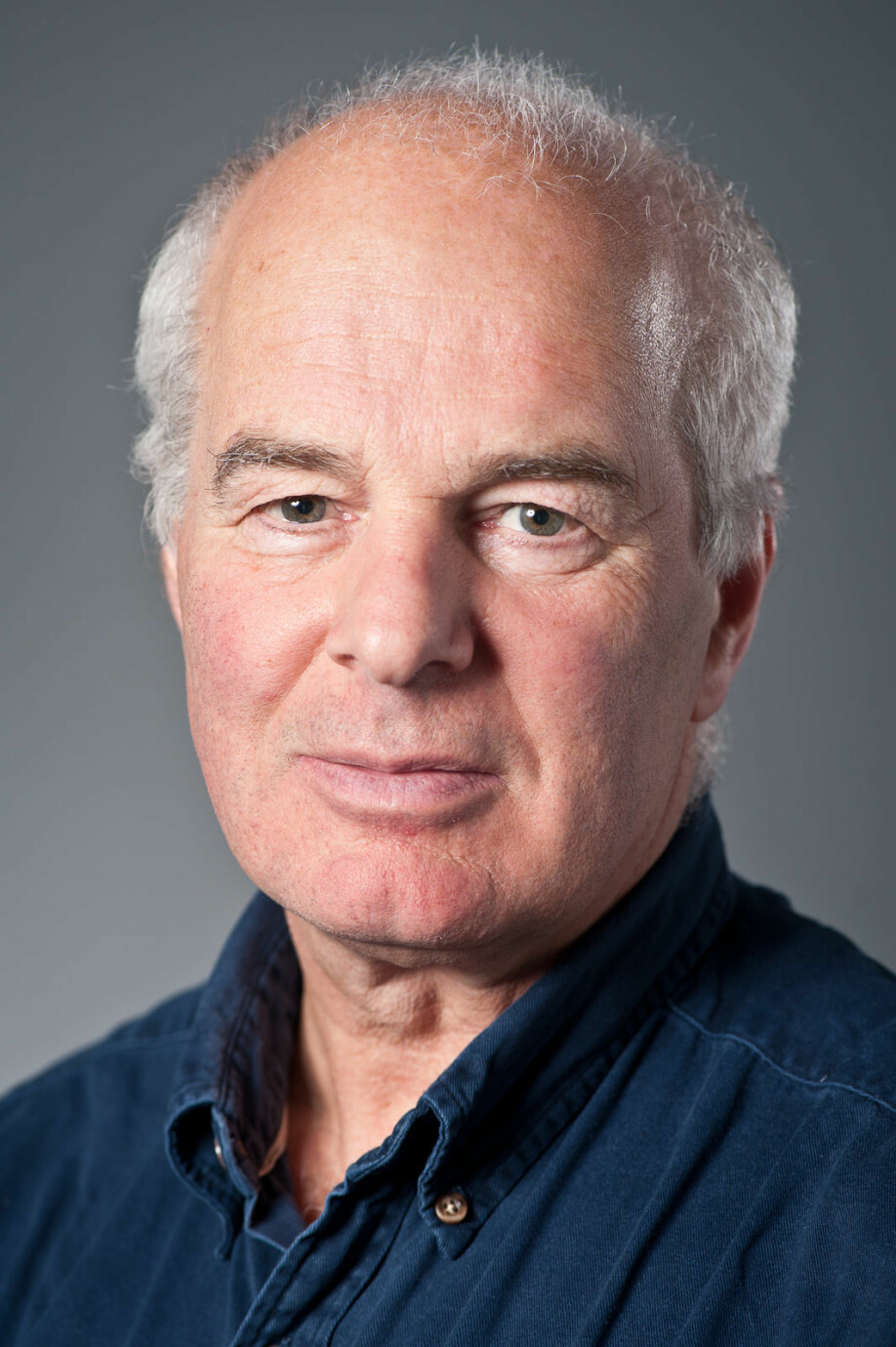
Ola Didrik Saugstad is a paediatrician and professor of paediatrics. His work includes research on ME/CFS. Saugstad is impressed with the researchers' work.”
“The study is very exciting and very thorough,” he says.
“I think you can even say that the study shows that this group is clearly in the international lead when it comes to ME/CFS research.”
Saugstad says he finds it particularly interesting that the researchers uncovered subgroups of ME/CFS patients.
He notes that the researchers’ 83 patients constitute a large body of material.
“Another positive about this study is that the patient participants are well defined,” he said.
Patients were diagnosed with ME/CFS according to the strict Canadian criteria.
“A lot of the ME/CFS research, especially from Norway, is controversial because the latest international definitions have not been used. But in this study they were,” says Saugstad.
Rejects myth
The study findings confirm what several researchers have believed, that ME/CFS patients have a disturbance in their energy conversion, says Saugstad.
“The study refutes the myth that nothing shows up in blood samples in ME/CFS patients. It’s true that if you go to your GP and get regular blood tests, you usually won’t find anything. But we’ve known for a long time now that you can see significant changes if you do special blood testing of ME/CFS patients. These tests reflect that their energy metabolism is poorer,” he says.
Then the question becomes what is the cause and what is the effect. One thing that can make it difficult to interpret results from ME/CFS studies is that the control groups do not allow for the possibility to control everything. Control groups that are as inactive as the ME/CFS patients are usually not available.
“Healthy controls were used in this study. A common objection is that ME/CFS patients experience these changes in metabolism because they’re inactive. That’s one argument,” says Saugstad.
In addition, questions also arise about whether the differences are specific to ME/CFS patients, or whether they are also present in other diseases.
Abnormal levels of lactic acid
Saugstad mentions a study led by Katarina Lien, where the researchers found that ME/CFS patients had an abnormally elevated level of lactic acid the day after they exercised.
“Lactic acid kicks in when you run 400-metres, or when you do anaerobic training and the muscles get too little oxygen. The body then makes less ATP, which is the body's fast energy reserve. The hypothesis that the cells of ME/CFS patients receive too little oxygen fits well with these findings,” says Saugstad.
Together with Swedish colleagues, Saugstad has just received support from the USA to measure the level of lactic acid and hypoxanthine in ME/CFS patients, as compared with healthy people. These are two biochemical indicators of oxygen deficiency. The study will be conducted in Sweden.
Tronstad explained that the lack of oxygen may involve the autoregulation of blood flow, which leads to the cells receiving too little oxygen during activity.
“The study hypothesis may be right. It’s always a question of chicken and egg and what comes first. But it’s conceivable that some mechanism could be contributing to ME/CFS patients' symptoms,” says Saugstad.
Translated by Ingrid Nuse.
Read the Norwegian version of this article on forskning.no.
References:
Fredrik Hoel, August Hoel, Ina K.N. Pettersen, Ingrid G. Rekeland, Kristin Risa, Kine Alme, Kari Sørland, Alexander Fosså, Katarina Lien, Ingrid Herder, Hanne L. Thürmer, Merete E. Gotaas, Christoph Schäfer, Rolf K. Berge, Kristian Sommerfelt, Hans-Peter Marti , Olav Dahl, Olav Mella, Øystein Fluge, and Karl J. Tronstad: A map of metabolic phenotypes in patients with myalgic encephalomyelitis/chronic fatigue syndrome, JCI Insight, 23 August 2021.
Øystein Fluge, Karl J. Tronstad, and Olav Mella: Pathomechanisms and possible interventions in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), Journal of Clinical Investigation, 15 July 2021.































