Non-invasive prenatal testing (NIPT) is now legal for all pregnant women in Norway. But how does it actually work?
How can a mother's blood test reveal a chromosome defect in the foetus? Knowing how the test works also makes it easier to understand why it doesn't always give an accurate result.
One of the changes in the Biotechnology Act passed in the Norwegian Parliament on 26 May is that noninvasive prenatal testing (NIPT) is now legal for all pregnant women in Norway.
This means that all pregnant women who want to check whether a foetus has certain chromosome abnormalities will soon be able to have this blood test in Norway, instead of going abroad to Sweden or Denmark, as many have done in previous years.
Under the previous regime, women aged 38 and over were offered the NIPT-test as they were defined as being in a higher risk group of having babies with chromosome abnormalities. This age limit is now lowered to 35. In addition, all other women can now take the test if they wish to do so. What this means isn't entirely clear yet, but doctors that the national broadcaster NRK have spoken to assume this means women younger than 35 will have to pay for the test themselves.
The changes in the Biotechnology Act also included that all women will now be offered what is called an early ultrasound - meaning an ultrasound done around week 12-13 of a pregnancy. 12 weeks is also the limit for self-determined abortion in Norway - after this, a woman has to have her case reviewed and decided by a tribunal.
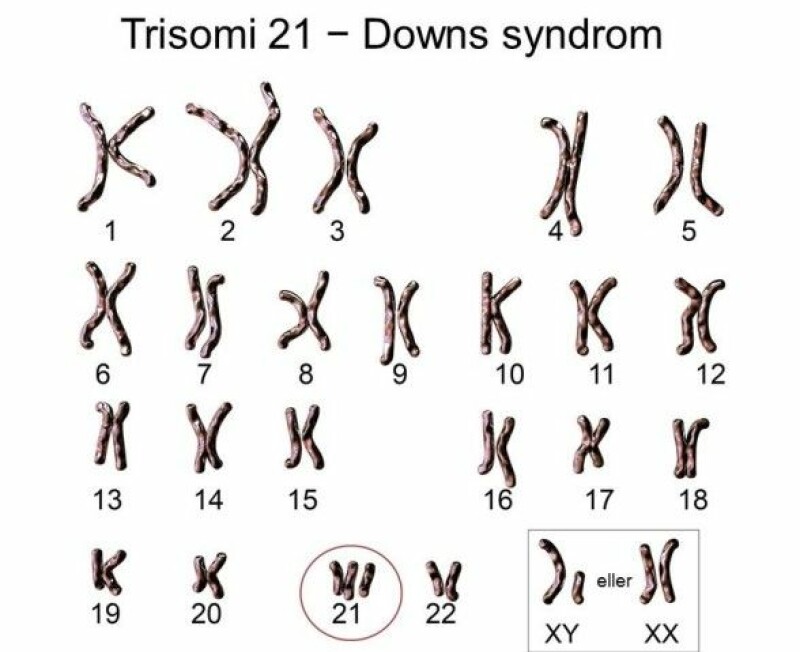
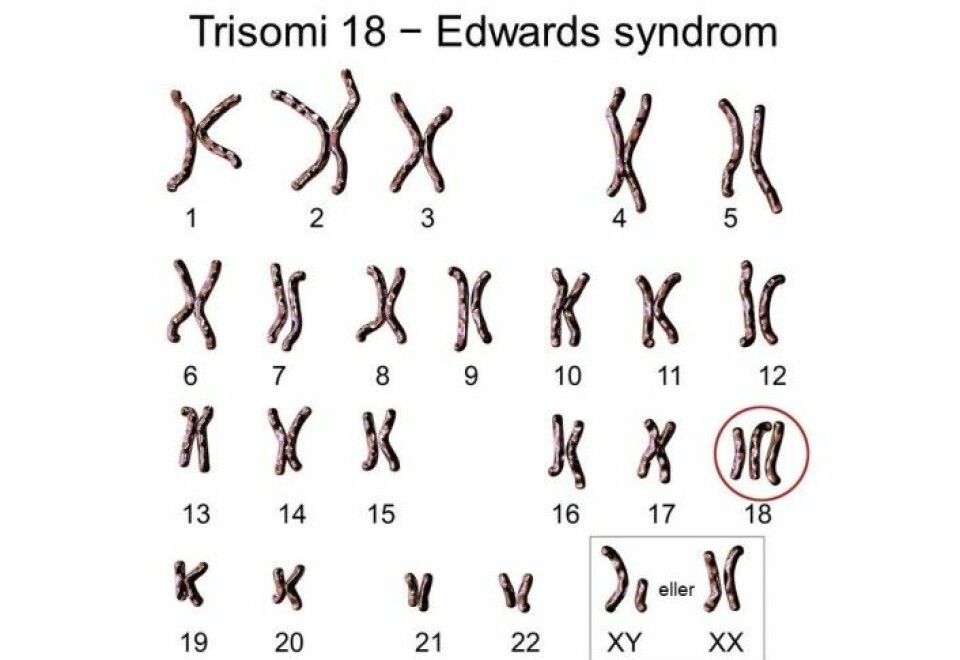
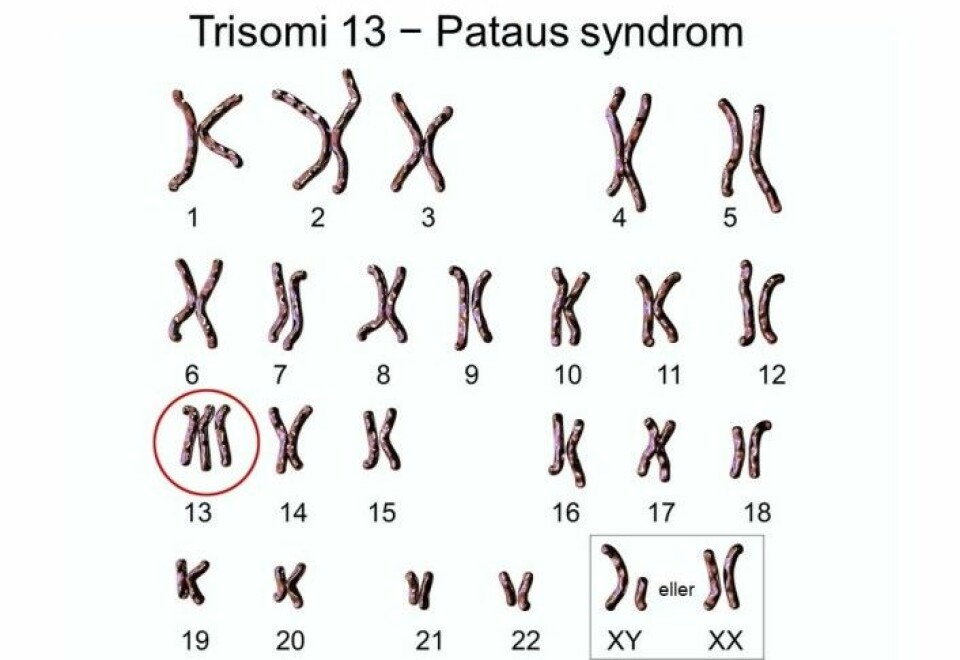
NIPT uses a blood sample from the mother that can detect the presence of an extra chromosome number 21, 13 or 18 in the foetus – otherwise known as Down syndrome, Patau’s syndrome and Edwards’ syndrome.
But how can a sample of the mother's blood tell us anything about the chromosomes in the foetus?
Doesn’t originate directly from the foetus
The test measures tiny bits of DNA found in our blood, says Caroline Bianchi Strømme, a senior adviser to the Norwegian Biotechnology Advisory Board.
“Our blood contains small fragments of DNA that circulate freely in the bloodstream. The free-floating fragments aren’t in cells and are therefore called cell-free DNA. They can arise from cells that have died,” says Strømme.
In a pregnant woman, some of this DNA has a different genetic code than her own.
So does it come from the foetus? Not really.
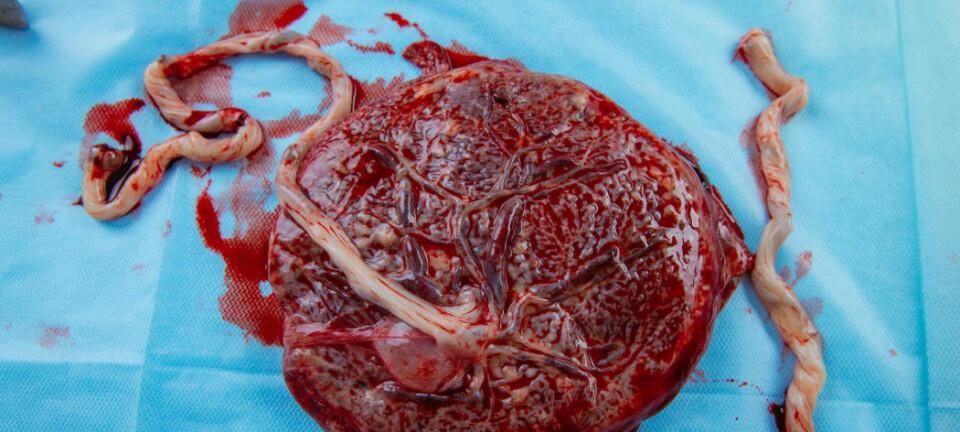
"This DNA actually comes from cells from the placenta, which has a DNA profile that is almost identical to that of the foetus," says Strømme.
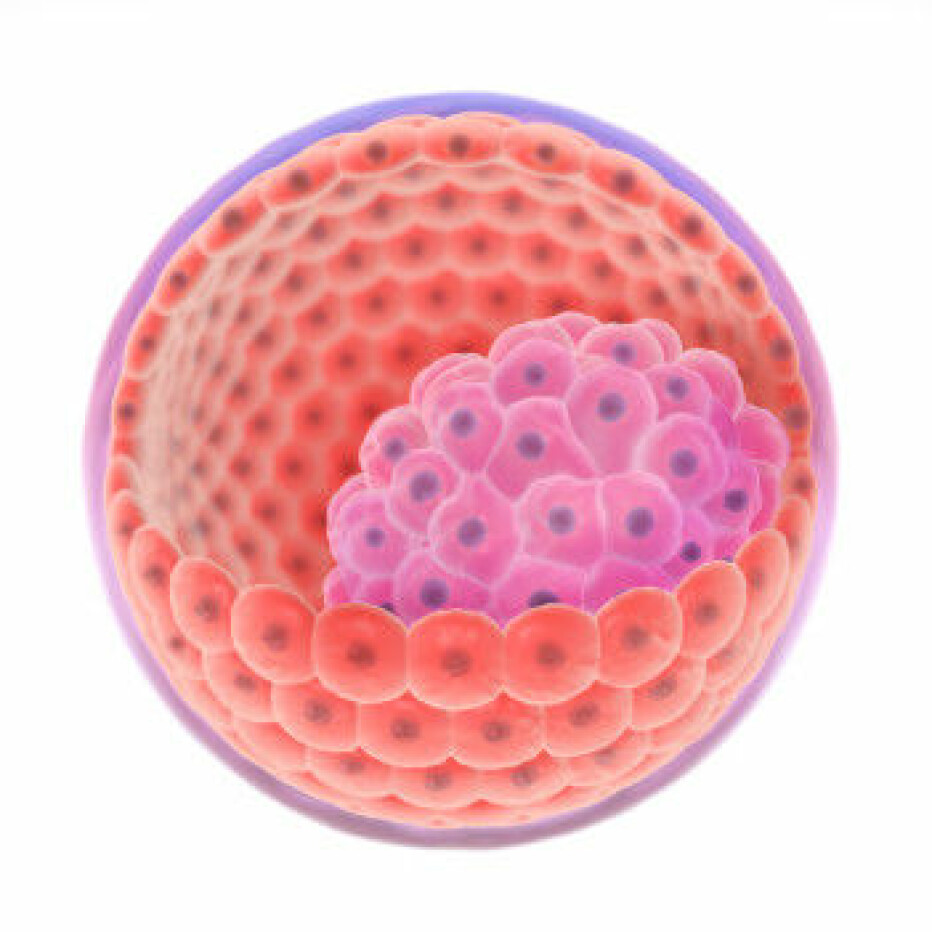
When the embryo is still just a small ball of cells, some of the cells start to specialize and develop into the placenta, while others become the foetus.
This means that the foetus and placenta usually have identical DNA, with genes from both mother and father.
Counts chromosomes
Technicians who analyse the NIPT blood sample can use DNA sequencing to measure the small pieces of DNA floating around in the blood.
They can also count the number of chromosomes that come from the placenta, according to Strømme.
Each cell in our body normally contains 23 pairs of chromosomes. Each of the 23 pairs includes one chromosome from the mother and one from the father.
Sometimes, two copies of a chromosome come from one of the parents. This is called a trisomy.
An extra copy of chromosome number 21 provides one of the least severe trisomies – Down syndrome. It is also the most common syndrome caused by having an extra chromosome copy.
Instances of having an extra copy of chromosomes 13 or 18 are far rarer, but are also much more serious conditions. Very few children with Patau’s or Edwards’ syndrome survive the first year of life.
Very precise, but not always
Some pregnant women have already undergone NIPT in Norway, because they had a greater risk of the foetus having chromosome disorders.
But the analysis itself has not yet been done in Norway, says Torbjørn Moe Eggebø, a consultant in foetal medicine at St. Olavs Hospital and a professor at NTNU.
So far the blood tests have been sent to Karolinska University Hospital in Stockholm to be analysed.
In a Norwegian article in Tidskriftet – Den norske legeforening (Journal of the Norwegian Medical Association), Eggebø presents the experiences this laboratory has with the test.
The figures so far show that NIPT captures nearly 100 per cent of cases with Down syndrome and Patau’s syndrome, and 95 per cent of Edwards’ syndrome cases.
But even though the test is very precise, false positive results occur in some of the pregnant women who actually have a healthy foetus.
Chromosome defects in placenta
One of the sources of error is that the test measures DNA from the placenta.
“Most of the time, the genetic material from the foetus and placenta is the same, but not always,” says Eggebø.
Some of the cells in the placenta may have an extra chromosome copy that does not occur in the foetus.
For example, parts of placenta may have a trisomy that arises after the cells begin to specialize as placenta cells.
Twin pregnancy is another reason NIPT may detect a defect when the foetus is actually healthy, Eggebø says.
The extra chromosome captured by the test could come from a deceased twin. In these cases, the deceased twin had a trisomy, but the surviving twin does not.
Therefore, a NIPT with a positive result for a trisomy should always be followed up with amniocentesis - which tests the amniotic fluid from the sac surrounding the fetus - in order to avoid unnecessary abortions, says Eggebø.
Qualified health professionals critical
That is one of the reasons why the people who administer the NIPT are qualified health professionals, says Eggebø. Women need to be thoroughly informed before taking the test.
He also thinks it is natural that the analyses of the blood tests should be done in Norway now that everyone can take the test in-country.
New ethical issues could also emerge.
The NIPT basically gives access to the entire genetic code of the foetus, says Strømme.
For now, only a limited list of conditions may be tested with NIPT in Norway.
But as the test becomes available to everyone, it will raise new ethical questions, says Norwegian Biotechnology Advisory Board leader Ole Frithjof Norheim.
Could detect more disorders
As DNA technology evolves, it will become technically possible to test for more conditions.
For example, the foetus may lack a small bit of a chromosome called a microdeletion, which can also cause various syndromes.
“NIPT has already been developed to test for some types of microdeletions,” says Strømme.
For example, some private clinics in Sweden already offer testing for DiGeorge's syndrome, where a small chunk of chromosome number 22 is missing.
Translated by Ingrid P. Nuse
———
Read the Norwegian version of this article at forskning.no