Fast or slow prostate cancer?
Some types of prostate cancer progress so slowly that the patient never requires treatment. The challenge now is to find out which patients need treatment and which don't.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Around 4,000 men in Norway are stricken with prostate cancer annually. This makes it one of the three most common cancers among the male population. Approximately 1,000 Norwegian men die of the disease every year.
But among the 4,000 men, many could go home from the doctor’s office with less worries after hearing the words: “You have cancer”.
Rolf Skotheim, cancer researcher and group leader at Oslo University Hospital and the Centre for Cancer Biomedicine, thinks far too many patients are unnecessarily burdened by cancer diagnoses that really won’t cause them any problem.
“Our challenge is to find out which patients actually need treatment.”
Men who live with prostate cancer
Skotheim cooperates in a group led by Ragnhild A. Lothe, who works at the Section for Cancer Prevention at Oslo University Hospital. They are searching for new biomarkers for prostate cancer and presenting their results recently at a prostate cancer conference in Oslo.
A biomarker shows there is a measurable change in a cell, indicating a potential danger.
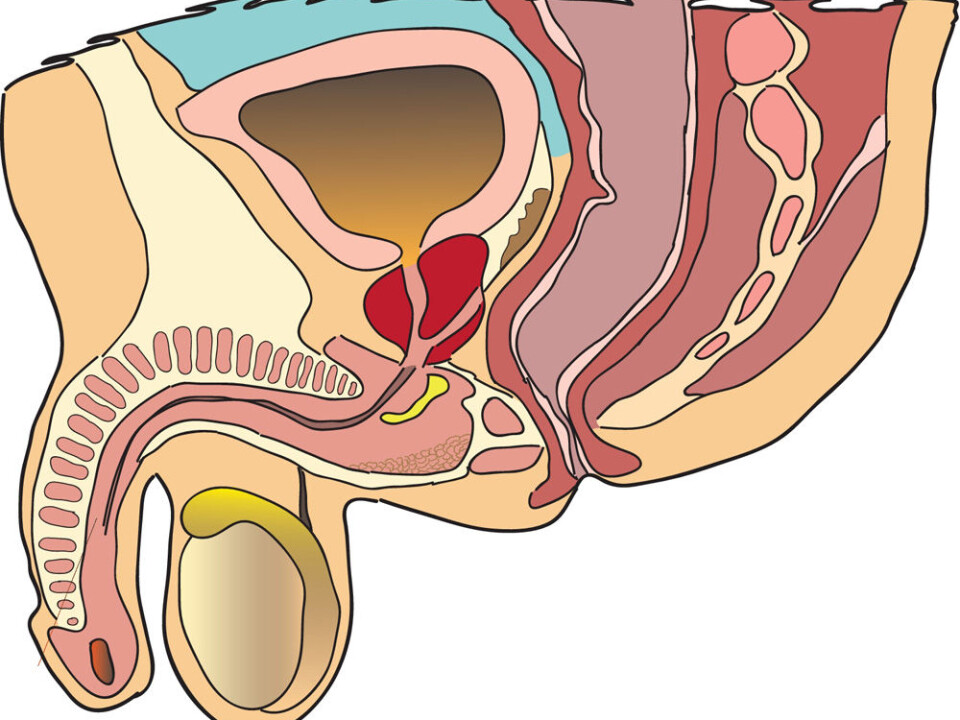
“The biomarker currently used to detect prostate cancer is called a prostate-specific antigen, or PSA. This is a protein that increases in the blood of a man with prostate cancer. But PSA doesn’t differentiate well between aggressive, dangerous cancers and slow-growing, non-dangerous types,” Skotheim explains.
Studies of gains from screening a population for abnormal PSA values have yielded some surprising results. If the population in one region are screened, and people in a neighbouring region are not screened, as you would expect more prostate cancers are detected in the first group.

But there was no more prostate cancer mortality in the region that hadn’t been screened. This means there are men who have prostate cancer, but who never get diagnosed or treated for cancer.
“This is confirmed by pathologists. When they are making their examinations of men who have died in accidents or from other diseases, pathologists often find that they had prostate cancer – but the patient never knew,” says Skotheim.
Statistics from the USA show that only 25-35 percent of men with elevated PSA values actually have prostate cancers.
Trauma could be averted
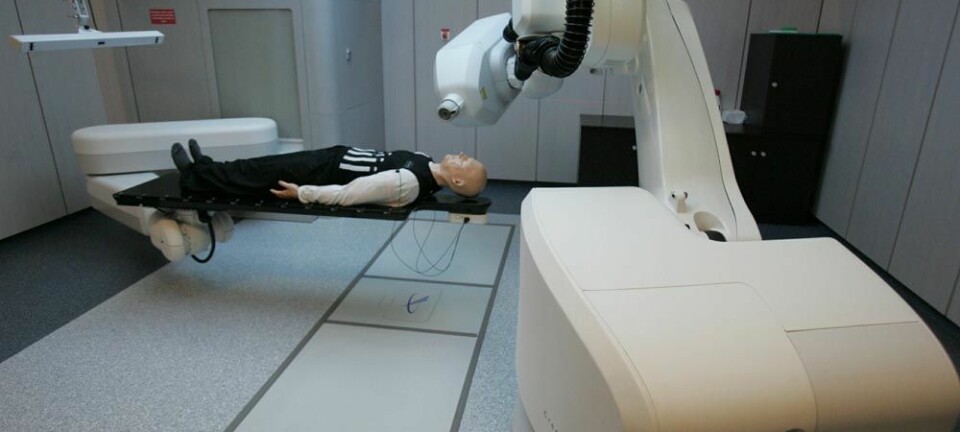
Prostate cancer is currently treated much like other cancers: operations, radiotherapy, and chemotherapy − and in some cases the removal of the testicles. The latter is to prevent testosterone production, because the hormone stimulates growth of prostate cancer cells.
All these forms of treatment are extensive and traumatic for the patients, as well as expensive for the national health services.
Skotheim says it would be a boon if diagnostics could sort out those who need treatment from those who can live well without it because their cancer is the kind that develops too slowly to cause a problem in their lifetimes.
“It’s just as traumatic for the patient in either case because we don’t know whether he needs treatment or not. This cancer is treated like any other because it is a real disease,” he points out.
Searching for foreign genes
Skotheim and his colleagues use modern genome technology, such as DNA sequencing, to find improved detectors for prostate cancer.
“What we’re really trying to do is find genes that are only present when the cancer is malignant. More specifically, we’re trying to find gene fusions, a special type of hybrid gene that is formed when genes on different chromosomes are broken and then reassembled inappropriately. If we find such gene mutations in blood or tissue samples, there is almost certainly such a cancer present,” he explains.
A number of researchers have worked the past few years on the issue of how over-expression of certain genes in cancer cells affects the disease.
"But when you try to use over-expression as biomarkers you get a lot of so-called false positives,” says Skotheim.
That means that the gene is hyperactive without it necessarily having anything to do with cancer. This is the problem with the present PSA test.
These over-expressed genes also had a function in the cell before a cancer started. This makes it hard to differentiate between a problematic hyperactivity and a natural elevated activity for a gene in a certain phase of life.
“On the other hand, gene fusions are genes in which the DNA has changed irreversibly; the DNA thread had been broken and reconnected in the wrong way. If you find these you usually know it isn’t good because that gene wouldn’t be present in healthy cells,” says Skotheim.
Help from knowledge of skin cancers
Gene sequencing, providing an understanding of which mutations and gene fusions present in bodies with a cancer, can also be used as an aid in treatment.
“We know about lots of genetic changes, and if certain mutation types are found in a patient, he will most likely respond to a special treatment. As time goes on we will become knowledgeable about more and more of these genetic changes, across a number of cancer types, enabling us to find treatment methods that work for more types of cancer,” explains Skotheim.
Researchers at the University of Michigan in the USA recently found a mutation in skin cancer, in which a gene designated as BRAF mutates in a special way. This mutation also turns up as a section of a gene fusion in some cases of prostate cancer.
That means the treatment for skin cancer with a BRAF mutation might also work for these prostate cancer patients.
Quick route to treatment
Mapping genes by sequencing or DNA has been demonstrated to be a relative efficient form of cancer research.
According to Skotheim, the discovery of the first gene fusion in prostate cancer was published in 2005 and although this gene isn’t used clinically yet, research is being conducted globally that seeks to use the gene to detect prostate cancer.
The same can be said regarding the BRAF gene fusion. If it turns out prostate cancer with this mutation reacts the same way as when the gene is mutated in a skin cancer, skin cancer treatment can be used on these prostate cancer patients.
“That treatment has already been cleared for use on human patients, so we have a chance of getting new treatment methods in just a few years,” says Skotheim.
---------------------------------------------------------------
Read the article in Norwegian at forskning.no
Translated by: Glenn Ostling
Scientific links
- N. Palanisamy et.al. (2010) Rearrangements of the RAF kinase pathway in prostate cancer, gastric cancer and melanoma. Nature Medicine, vol 16, no. 7, pp 749-750(Abstract)
- National Cancer Institute: Prostate-Specific Antigen (PSA) Test