New cancer drug shows great promise
A new drug for cancer treatment is making good headway. “We’re getting close to our goal,” say scientists.
Danish and American scientists have developed a new drug against prostate cancer.
The cornerstone of the new cancer drug is the substance thapsigargin, which is extracted from the Thapsia garganica, a plant that grows in the Mediterranean.
The scientists are currently trying to get mosses and yeast to form thapsigargin, which would provide sufficient amounts of the substance to produce the cancer drug on a large scale.
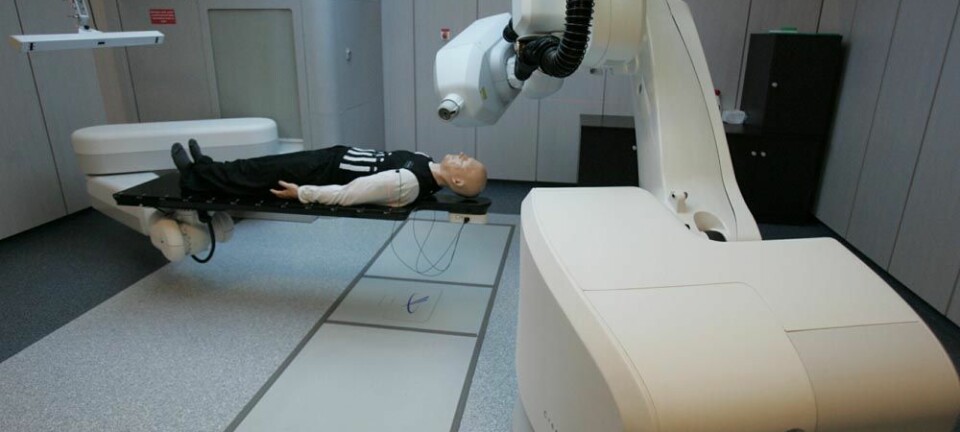
The drug is currently being tested on humans, and success in these trials could open up for entirely new opportunities in the fight against incurable types of cancer.
The findings have just been published in the journal Science Translational Medicine.
“It’s nice, for once, to be able to say that we’re getting close to our goal when it comes to developing new drugs against cancer,” says Poul Nissen, a professor in Protein Biochemistry at Aarhus University, who has developed the new drug together with his Danish colleagues and scientists from Johns Hopkins University and oncology company Genspear in the US.
He says that the new drug has shown very promising results in animal tests, and if the results can be recreated in humans, it could well develop into a medicinal product and a brand new method for future cancer treatment.
“Developing medicine at the atomic level is a lot like playing with Lego bricks,” he says. “We look at how the drug works and then we can manipulate various functions that further improve the drug. This has enabled us to create a drug that acts on types of cancer that we previously couldn’t do anything about.”
Makes cancer commit suicide
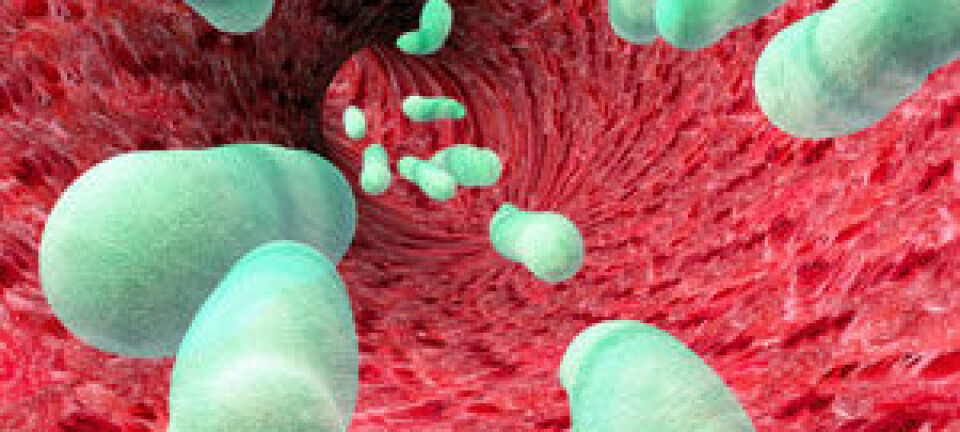
Central to this new treatment is the fact that all cells have a need to control the levels of calcium in the cell and in its various subunits, known as organelles.
If the cells are unable to control the calcium levels, certain mechanisms within the cell are activated, which eventually causes it to commit suicide.
This is the body’s natural defence against, for instance, damaged cells which could potentially develop into cancer. This is why calcium signalling has long been a target mechanism for cancer researchers.
Calcium is one of the key substances in the cells’ regulation of various enzymatic processes. When the cell discovers that its calcium level is out of control, it ends up killing itself, explains the professor.
“The new drug – G202 – is designed to destroy the calcium regulation specifically in cancer cells by feeding them the poisonous thapsigargin and that way getting them to kill themselves.”
Aggressive cancer opens the door to a new form of medicine
Control over the calcium concentration is central to all cells in the body, not just cancer cells. Simply giving cancer patients a substance such as thapsigargin is not a good idea, since doing so would cause many other cells in the body to die.
As a result, the researchers have developed a method of targeting cancer cells directly.
This is where prostate cancer showed the way.
Cancer cells form a host of aggressive enzymes known as proteases (see Factbox) to destroy and transform the surrounding tissue. Generally speaking, cancer cells do this in order to create more space for further growth.
“This gave us the idea of placing thapsigargin on tiny pieces of proteins that are the target for destruction in these cancer cell proteases. The result was the drug G202,” he says.
“The G202 molecule is so large that it cannot enter the cells, which means it doesn’t damage the body. But when G202 comes close to a prostate cancer cell, the proteases cut the protein segment of the molecule into pieces, thus releasing thapsigargin.”
Once the thapsigargin has been released, it will rapidly penetrate the nearest cells, i.e. the cancer cells.
“In so doing, G202 only hits prostate cancer cells, leaving the body’s own cells unhurt. The cancer cells will simply suck it up and prepare for their own death,” says Nissen.
Works against other cancers too
Since the G202 could potentially be cut by several cancer cell types, the new drug is expected to be able to attack other types of cancer than just prostate cancer.
The protease that cuts the G202 molecule is also present in the new blood vessels formed by cancer tumours in order to ensure the supply of nutrients to the newly-formed cancer cells.
Besides prostate cancer, this also applies to cancer types such as breast cancer and bladder cancer.
The drug can therefore also be cut in these surrounding blood vessels, and the cancer tumours – in addition to killing themselves by suicide – are suffocated due to a lack of blood supply.
This means that the drug may well be effective against several types of cancer.
The entire molecular puzzle regarding the coupling of thapsigargin to proteins has mainly been the responsibility of Søren Christensen Bragger, a professor with special responsibilities at the Department of Medicinal Chemistry at the University of Copenhagen.
G202 puts calcium pumps out of action
The calcium levels in the cells are controlled by various pumps in both the outer and inner membranes.
The outer membrane pumps regulate the basal calcium levels in the cell, while the internal pumps, such as the calcium pump SERCA, maintain the internal calcium storages. SERCA does this by pumping calcium from the cytoplasm into the storages, thus increasing the calcium levels.
It is this SERCA pump that the G202 trial drug targets.
The functional part of the drug – thapsigargin – is capable of blocking SERCA, so that calcium slowly leaks out into the cytoplasm but is not pumped back, which eventually starts the suicide process that kills the cancer cells.
------------------------------
Read this article in Danish at videnskab.dk
Translated by: Dann Vinther