Here’s how more precise radiation can reduce side effects for cancer patients
Statisticians in Bergen have developed a more personalized approach to radiation therapy that over the long run will reduce side effects in cervical cancer, rectal cancer and prostate cancer.
More and more people are surviving cancer, with better treatments accounting for much of this improved survival. More than half of cancer patients receive radiation therapy as part of their treatment. Every day, radiation helps heal a large number of cancer patients.
Nevertheless, the treatment can be made even better, researchers have found.
Radiation treatments for cancer in the pelvic area can cause damage to the intestinal system and affect potency. This applies to cancers such as prostate cancer, cervical cancer and rectal cancer.
Researchers in Bergen, Norway, have now developed a more personalized plan that over the long run can reduce the side effects of radiation treatment.
Fine balancing act

The goal of radiation therapy is to destroy the entire tumour, while damaging as little of the healthy tissue around it as possible. But this isn’t easy.
Tightly targeting radiation therapy in the pelvic area can be very challenging.
If radiation therapists irradiate healthy tissue around the tumour, the patient will develop side effects, such as diarrhoea, or problems controlling their bladder or intestines.
Radiation in the pelvic area can also damage sexual function. Women can develop pain during intercourse and men can have problems with potency.
On the other hand, if therapists don’t radiate a big enough area, they won’t destroy enough of the tumour to knock it back.
Researchers in Bergen have now developed an approach that uses statistical calculations and 3D images of prostate cancer patients to calculate a more precise area to be irradiated.
Damages less tissue than before
To be on the safe side, the therapists irradiate both the tumour and a safety margin around it.
“In the past, a much larger area has been irradiated than needed,” Liv Bolstad Hysing told sciencenorway.no. She is a project manager and researcher in medical physics at Haukeland University Hospital.
But there have been tremendous developments in recent years, she says.
“Now we take daily pictures so that we damage less healthy tissue than before,” she said.
The safety margin that is irradiated has been reduced from a few centimetres to a few millimetres in some patient groups. This is particularly true for prostate cancer, where gold markers can be implanted in the prostate to help target radiation.
The researchers reported their improvements in prostate cancer treatment in June last year.
But the goal of the new research is to be even more accurate for all patient groups who have to have radiation therapy in the pelvic area.
Organs can move around
Patients are irradiated based on a plan that is crafted before treatment begins. The plan includes the area to be irradiated and areas that need to be protected.
For most people, the plan remains unchanged throughout the course of treatment.
The plan is based on CT images of what the patient’s pelvic area looks like before the treatment starts, and with a safety margin that is the same for all patients.
But this has obvious drawbacks. First, people are very different.
“Some people are more flexible in the pelvic region than other people, which means that their organs can move more than in other patients,” Hysing said.
The diseased area may shift
In addition, the location of the organs, particularly the bladder and intestines, may vary from day to day in a single patient.
“This depends on how full your bladder is or how much food you have in your gut, based on your digestion and what you have eaten and drunk. These natural changes from day to day move the area around the tumour and constitute the biggest challenge,” she said.
In the radiation treatment of the future, therapists will be able to take these changes into account better than they do today.
“Manufacturers are making progress in developing new radiation machines that will make this possible in the next few years,” she says.
The interdisciplinary research group that Hysing heads is working to develop better methods that can be used on the new machines.
More individual plan with statistics
Researchers at Haukeland University Hospital, in collaboration with the University of Bergen and NORCE, have now developed a more accurate model for this newer type of radiation treatment.

Their advanced statistical model is designed to provide a more realistic description of how the organs move in the pelvic region, and has been developed by Øyvind Lunde Rørtveit, a PhD candidate at Haukeland University Hospital.
The model is based on 300 CT images of previous prostate cancer patients, taken during treatment. The images allowed the researchers to see how the organs changed shape and location internally during the course of the treatment.
They then compared and adjusted this information using images of each patient.
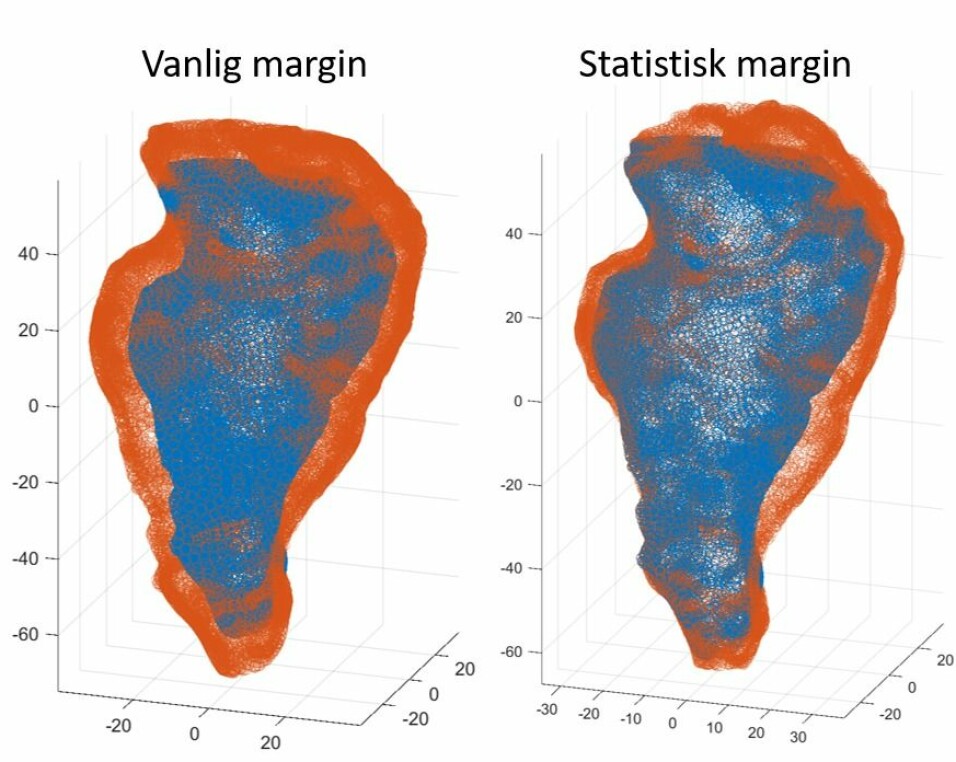
“This allows us to create a more individualized plan for the size of the area to be irradiated,” said Andreas S. Stordal at NORCE, the Norwegian Research Centre. Stordal is one of Rørtveit's supervisors.
Estimates show that this more-individualized approach can provide a 20-25 per cent improvement in the volume that should be irradiated, so that the damage is reduced, Stordal said.
The researchers have only worked with images of prostate cancer to date.
But in the long run, the method can also be used for cervical and rectal cancer to reduce side effects.
Can protect more healthy tissue
The usual approach to treating cancer patients with radiation is to expand the clinical area to be irradiated with a safety margin, to compensate for uncertainties related to the size and location of the tumour.
However, this method does not differentiate between how much movement there may or may not be in each patient’s organs in the pelvic area.
“The more person-specific treatment we can create, the less the risk of irradiating healthy tissue,” says Hysing.
But at least as important as reducing the irradiated area is that this more-personalized treatment allows clinicians to increase the radiation dose used on the tumour. Currently, doctors now have to keep doses low because they are also irradiating a safety margin outside the tumour.

“By adjusting the area that can be irradiated more individually, you can increase the dose,” Hysing said.
Radiation therapy is teamwork
Radiation therapy requires interdisciplinary collaboration, where medical physicists are responsible for ensuring that the treatment prescribed by a doctor is actually provided.
The doctor orders the treatment and radiation therapists work on the machine and undertake the treatment.
Medical physicists work more behind the scenes but are central in the development and quality when it comes to new treatment methods in the hospital.
Gearing up for a new proton therapy machine
This project has required cross-disciplinary research between radiation and proton therapy, statistical modelling and algorithm development.
The results were supposed to be presented at a Nordic conference this spring, but the conference was cancelled due to the coronavirus pandemic.
Nevertheless, “we have a long way to go before this is used in clinical treatments,” Hysing said.
Haukeland University Hospital has recently ordered a new machine that allows radiation treatment using photons. It will be available for use in Norway from 2023-2024.
The project is in part designed to prepare radiation therapists for the new proton therapy facility.
Proton therapy is a more precise form of radiation.
Today, proton therapy is used primarily for the treatment of tumours that stay still, because it is more sensitive to shifts in anatomy than current treatment. The new method may also make proton therapy available to patients with tumours in the pelvis.
Translated by: Nancy Bazilchuk
References:
S. Thörnqvist et al.: Adaptive radiotherapy strategies for pelvic tumors – a systematic review of clinical implementations. Acta Oncologica, 8 April 2016.
L. Hysing et al.: Statistical motion modelling for robust evaluation of clinically delivered accumulated dose distributions after curative radiotherapy of locally advanced prostate cancer. Summary. Radiotherapy and Oncology, August 2018.
C. Ekanger et al.: Ten-Year Results From a Phase II Study on Image Guided, Intensity Modulated Radiation Therapy With Simultaneous Integrated Boost in High-Risk Prostate Cancer. Advances in Radiation Oncology, May - June 2019.
S. Pilskog et al.: Plan Selection in Proton Therapy of Locally Advanced Prostate Cancer with Simultaneous Treatment of Multiple Targets. International Journal of Radiation Oncology Biology Physics, 1 March 2020.
———