New test method for prostate cancer lowers the risk of infection – making antibiotics unnecessary
Men who are examined for possible prostate cancer run a high risk of infections. A new way of taking tissue samples via the skin can make the use of antibiotics redundant, a Norwegian study shows.
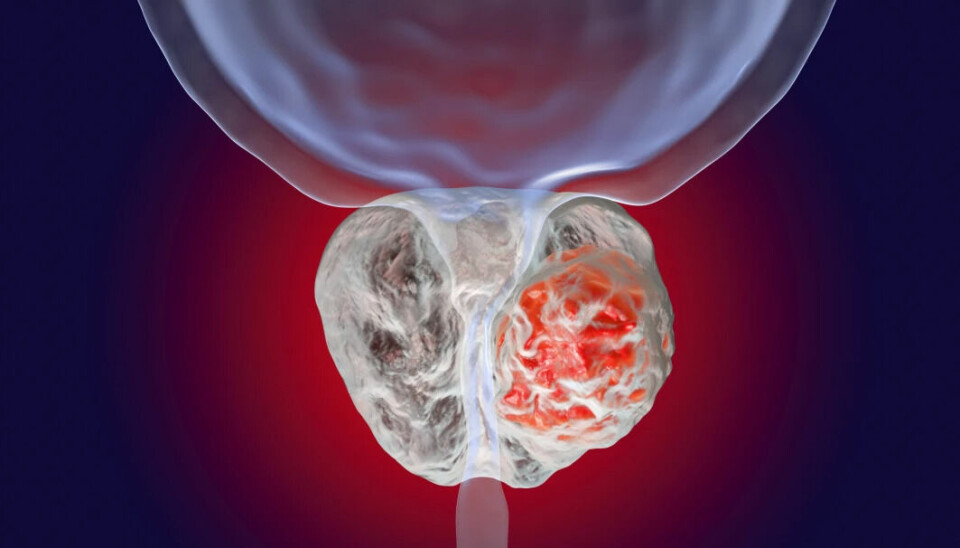
In circumstances where prostate cancer is suspected, tissue samples are taken from the prostate. The traditional method in which this is done poses a risk of infection.
Therefore, all patients are given antibiotics first, to prevent infections and sepsis.
A new method allows tissue samples to be collected in a more sanitary way. The new Norwegian study shows that this method can be implemented without the use of antibiotics. The study was recently published in the journal The Lancet Infectious Diseases.
Biopsy if cancer is suspected
If it is suspected that a patient has a diseased prostate gland, the first step is to take a blood test. Prostate-specific antigen, PSA, increases markedly in those with a diseased prostate.
Next, the patient is examined with an MRI.
But to determine whether the patient has cancer or not, the doctors must take a biopsy – a tissue sample – of the prostate.
This is usually done via the lining of the rectum.
“It is an unhygienic procedure which puts the patients at risk of urinary tract infection,” doctoral candidate Maciej Jacewicz at Oslo University Hospital (OUS) tells sciencenorway.no.
As many as five to seven per cent of men get an infection afterwards, according to previous studies.
The incidence of sepsis is between 0.3 and 9.4 per cent.
Antibiotics are therefore given in advance of the procedure.

New method extracts tissue via the skin
A new method involves taking prostate tissue samples through the skin in the perineum instead. It results in lower infection rates and a very low incidence of sepsis.
A needle is inserted through the skin in the area between the rectum and the scrotum.
The patient is given local anaesthetic, the skin is sterilised and, if necessary, shaved.
Previous studies have shown that cancer is detected just as effectively with this method as with the traditional method currently in use.
Nevertheless, not all Norwegian hospitals have adopted this new method.
The European Association of Urology recommends switching to the new biopsy method.
May reduce antibiotic resistance
“The study shows that the infection rate in those who did not receive antibiotic prophylaxis was not higher than in those who received antibiotics,” Dag Berild, professor of medicine and specialist in infectious diseases, writes in an e-mail to sciencenorway.no.
Through his research, Berild has contributed to putting the threat of antibiotic resistance on the agenda.
“Based on the large number of people who get this form of prostate biopsy, this study can contribute to a reduction in the use of antibiotics and thus a reduction in antibiotic resistance,” he says.
Will phase out old method
Doctoral fellow Maciej Jacewicz at OUS has carried out the study, together with colleagues in Oslo and in Germany. He works at the urology department at OUS.
“Our study of over 500 men shows that preventive antibiotics are unnecessary in patients who do not have an increased risk of infection,” Jacewicz says.
“Our wish is to phase out the old method and put an end to unnecessary antibiotic use in connection with diagnosing prostate cancer,” he says.
He is now completing his doctorate on the subject.
Still give antibiotics
“Although this new biopsy method is much more hygienic, it is still routine to give patients antibiotics to prevent infection,” says Jacewicz.
Other studies have also shown that the risk of infections is low. But this is the first randomised study that confirms that preventive antibiotics are unlikely to be necessary.
Three men out of 276 who did not receive antibiotics did indeed get an infection, compared to one in the control group who received antibiotics.
“But no one became seriously ill and had to be hospitalised. They got mild infections for which they were treated with a course of tablets,” he says.
Only four out of 555 men got a milder infection. This corresponds to 0.7 per cent.
“This study thus proves that it is redundant to give preventive antibiotics when using this new method,” says Jacewicz.
According to European guidelines, antibiotics must be administered anyway.
A great impact on many
Just over 5,000 men are diagnosed with prostate cancer in Norway each year.
Taking a biopsy of the prostate is one of the most common procedures in urology and affect many men every year.
In Europe and the USA alone, approximately two million such biopsies are performed each year.
“Prostate biopsies therefore have a major impact on very many men, and many who get an infection do not even have cancer,” Jacewicz says.
Therefore, it is high time to adopt the new method throughout the country, he believes.
Antibiotic resistance
Increasing antibiotic resistance in the world means that the healthcare system must try to reduce unnecessary antibiotic use.
Total consumption of broad-spectrum antibiotics in Norwegian hospitals was reduced by 11.8 per cent from 2012 to 2021.
But consumption was higher in 2021 than it was in 2020 and 2019, the national competence service for antibiotic use in the specialist health service (KAS) reported in March.
Admittedly, antibiotic resistance in Norway is relatively low. But in several other European countries, resistance is so high that many forms of antibiotics do not work.
“Those who undergo a biopsy are often given broad-spectrum antibiotics over several days. This is extra worrying when there is no increased risk of infections associated with the new method,” says Jacewicz.
Strong support for change
“Our results will hopefully lead to patients not being exposed to a procedure where there is a high risk of infection,” he says.
Hopefully the old method will be phased out.
Ola Bratt at the University of Gothenburg writes in a commentary in Lancet Infectious Diseases that the results of the study are significant enough to support a change in methods.
“Consistent results from at least two randomised trials are usually required to change a clinical practice,” he writes.
But since the same low infection rates have been shown in eight studies with more than a thousand patients, he believes the results are strong enough to support a change.
———
Translated by Alette Bjordal Gjellesvik.
Read the Norwegian version of this article on forskning.no
References:
Jacewicz et al. ‘Antibiotic prophylaxis versus no antibiotic prophylaxis in transperineal prostate biopsies (NORAPP): a randomised, open-label, non-inferiority trial’, Lancet Infectious Diseases, 2022. DOI: 10.1016/S1473-3099(22)00373-5 Summary.
Jacewicz et al. Cancer Detection Rates in Targeted Transperineal MRI-TRUS Elastic Fusion-guided Prostate Biopsies Performed Under Local Anesthesia, Anticancer Research, 2021. DOI: 10.21873/anticanres.15244
































