Share your science:
A bright spot in the fight against prostate cancer
SHARE YOUR SCIENCE: By combining different imaging techniques for scanning organs in the body, we can discover relapse of prostate cancer more easily.
In nearly 2 out of 5 cases of prostate cancer, the cancer returns. It may however take 7 to 8 years from a suspected relapse is discovered on a blood test until we can uncover the location and severity of the relapse by using traditional imaging modalities like MR and CT. With the relatively new imaging method PET/MR, we can 'see' the cancer much earlier – and perhaps more clearly. This is literally a bright spot in the fight against prostate cancer.
Tracing the prostate
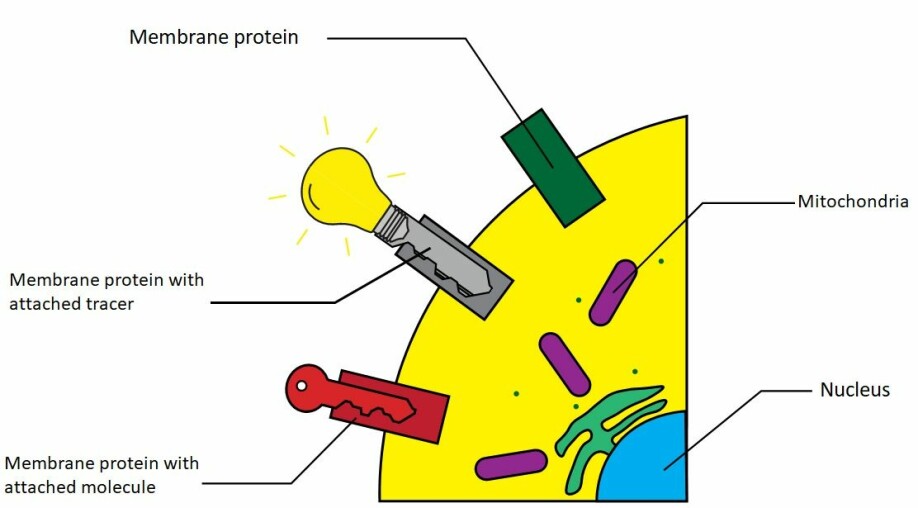
Positron emission tomography (PET) works by injecting the imaged patients with a medicine that has been labelled with a radioactive isotope. This isotope emits light as it decays, and thus acts as a 'light bulb', which can be seen with the PET-machine. Where many of these light bulbs are gathered, we will see bright spots in the resulting images. When such a 'light bulb' is attached to a medicine, we call it a tracer.
Tracers are small amounts of carefully chosen substances that have been radioactively labelled. We can think of a tracer as a key with an attached light bulb. This key can be designed so that it attaches and locks itself to specific types of cells which in turn will 'light up' when an injected patient is placed in a PET-machine.
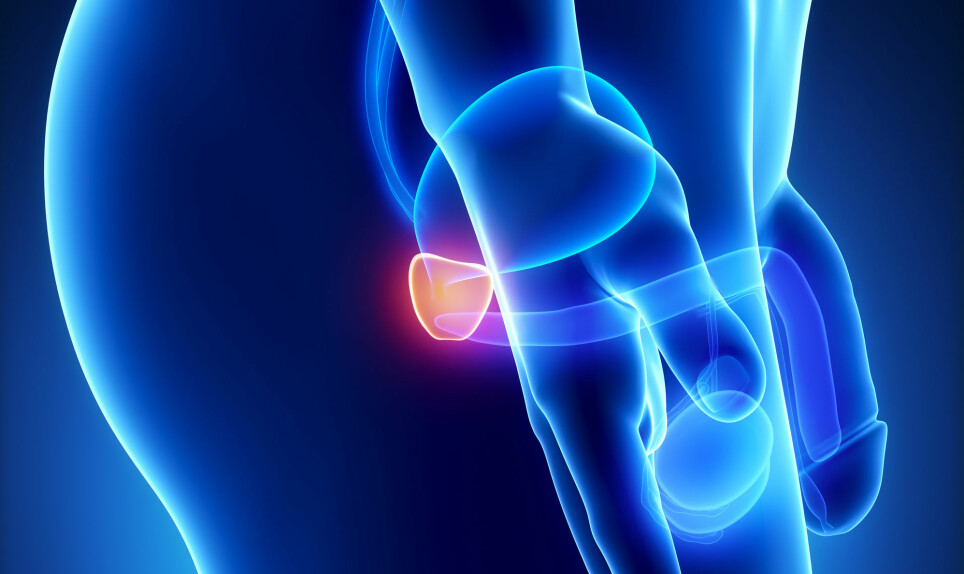
Prostate specific membrane antigen (PSMA) is a revolutionary tracer. As the name suggests, this tracer attaches itself to prostate tissue (and a select few, other tissue types). As the prostate in and of itself is not too hard to recognize on traditional imaging modalities you may ask what is useful about this? Common treatment for patients with prostate cancer without metastasis is to remove the prostate gland. After this there should be no prostate tissue left. If, however, we see that the prostate tracer finds and attaches itself to tissue in the prostate bed, where the prostate used to be, or in the surrounding area– especially lymph nodes – this is often an indication of a relapse.
PET in combination with prostate tracers therefore help us give an early diagnosis and provide further treatment to patients experiencing relapse. We can find metastasis in the lymph nodes or local relapses no bigger than a few millimetres – so small that they cannot be distinguished from normal tissue on conventional MR or CT imaging.
The PET images do not provide information on the surrounding organs
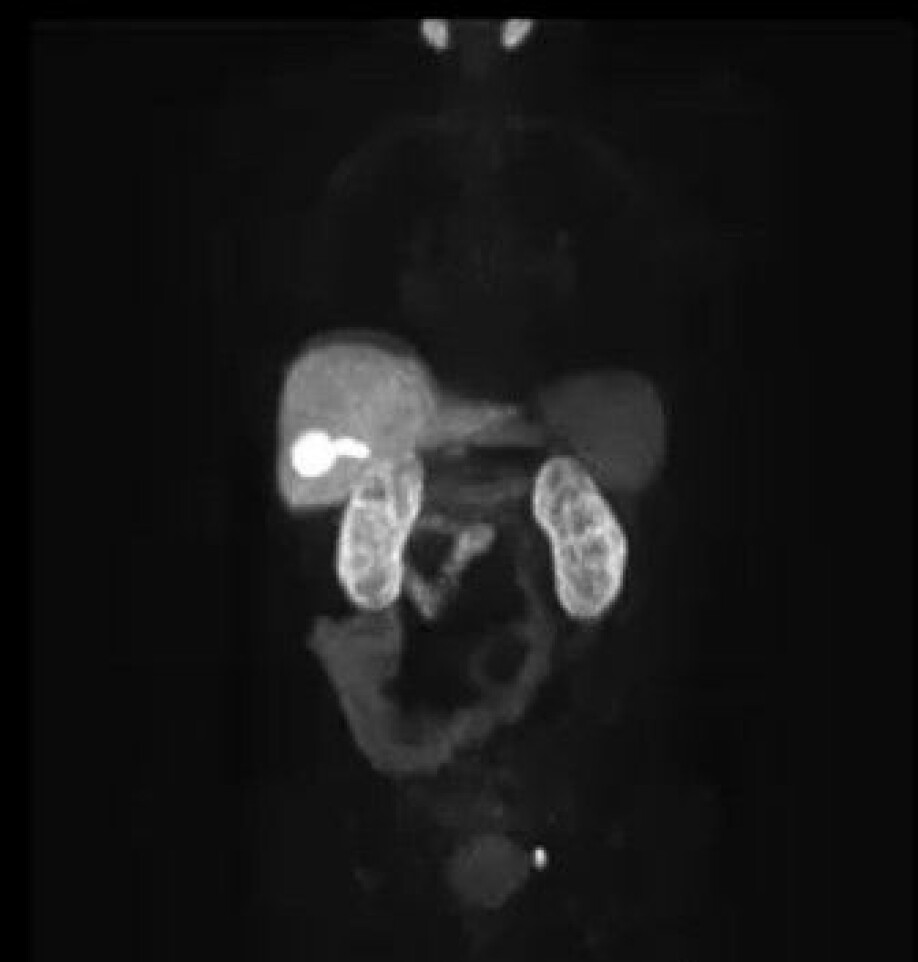
Although this may sound fantastic, PET alone is of little use. In this case, PET looks like a dark image with bright spots where the prostate tracer has attached itself. It is comparable to a satellite image of the Earth at night. The cities light up, but it is not so easy to distinguish mountain from plain – or land from sea. In a similar manner, the PET images do not provide any information about the 'landscape' where the prostate tracer has attached itself. The PET images are therefore almost always taken together with CT or MR, which provide information about the body’s structures and 'landscape' – that is to say, the anatomy.
PET combined with CT, is the most common hybrid modality in use today. Here the CT images are used both for the anatomical information they give and to correct the PET image itself. The correction is a so-called transparency correction. We are not able to catch all the light that comes from the prostate tracer. The light is dimmed when passing through the body on its way to the detectors in the PET machine, and what lies between the tracer and the detector determines how much of the light we are able to detect.
We can think of the body as a fog between the tracer and the detector: Where there are bones, the fog is thick and where there is soft tissue, it is more like a thin haze. To make the PET images give a correct representation of how the tracer has spread through the body, we need to 'remove' the fog. The information on how we do this, is exactly what we get in a CT image.
The CT images are good at distinguishing between tissues based on density, like for example lung and bones, but is poor at distinguishing between different kinds of soft tissue such as fat and muscle. This, however, is one of MR’s strengths, and this is important as the pelvic region largely consists of soft tissue. In clinical practice it is therefore common to take MR images in addition to the PET/CT images when relapse is suspected.
Pros and cons
By using PET images combined with MR images, the patient does not have to be imaged in two different machines. For the patients this means less time in the scanners, and less radiation. This is especially important considering that there can be many examinations over the course of cancer treatment and subsequent monitoring.
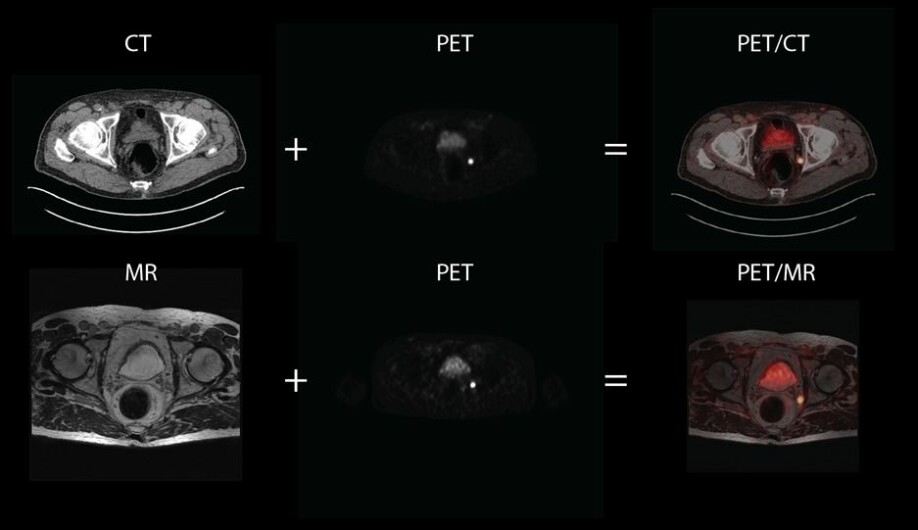
With these images, we nevertheless have a great disadvantage: we cannot use the MR images to 'remove the fog' from the PET images in the same way as we did with the CT images for PET/CT scans. To do this, the MR images must be 'translated' to the corresponding CT images – which is very difficult to achieve.
Although the MR images in this case are more useful than CT images by themselves, the PET images are potentially poorer for combined PET/MR imaging than for combined PET/CT imaging. We are currently uncovering exactly how good the images from PET/MR are in comparison with PET/CT for prostate cancer examinations. We are also working on finding new and better ways to improve PET/MR by using artificial intelligence and smart use of the information contained in the MR images. With these improvements we hope to be able to give tomorrow’s prostate cancer patients more reliable, less painful, and earlier diagnosis when relapse is suspected.
———
Read the Norwegian version of this article at forskning.no
Share your science or have an opinion in the Researchers' zone
The ScienceNorway Researchers' zone consists of opinions, blogs and popular science pieces written by researchers and scientists from or based in Norway.
Want to contribute? Send us an email!




























