What is going on in the bodies of ME/CFS patients?
Chronic fatigue syndrome remains a mystery. Many factors likely contribute to triggering and maintaining the problem. Here we take a closer look at what recent research has found out about biological differences between healthy people and ME/CFS patients.
Chronic fatigue syndrome (CFS) – also called myalgic encephalomyelitis (ME), or ME/CFS – is a difficult disease.
Patients report major physical problems: Even the slightest effort drains their energy for days. They experience flu symptoms and sleep disorders. Their body aches, their pulse rages and their head is in a fog.
Yet, when doctors examine them, they find nothing. Blood tests and MRI and CT scans are mostly normal.
Research has begun to reveal a new picture. As researchers are able to look at our biology more deeply and with greater precision, one deviation after another emerges in several of the body's important systems.
The question now is:
How are we to understand this complicated picture?
Why don’t all patients show the same changes? Are the changes just a consequence of the disease? Or do they signal causal mechanisms? And how might all the different discrepancies be linked?
ScienceNorway.no set out to learn more about what we do and do not know about what happens in the body of people with ME/CFS.
Scant research
The available research on ME/CFS is limited.
ME/CFS research is underfunded relative to the disease burden in the population, especially in biomedicine, according to an American study in the journal Work.
A search of the Pubmed research database confirms this. Keywords multiple sclerosis or schizophrenia show that at least ten times more studies have been published on these diseases, and over 20 times more studies with the keyword diabetes 1, than on ME/CFS in the last year. All these diseases affect about the same number of people.
However, the situation is improving. Several researchers are taking action, and certain developments are also making it easier to find answers.

Sharper criteria and better technology
In 2015, researchers at the Institute of Medicine (IOM) (now the National Academy of Medicine), developed clearer criteria for recognizing ME/CFS.
These criteria make it easier to distinguish ME/CFS from other disorders that cause fatigue.
New tools and methods are also enabling researchers to look more deeply into genes, intestinal flora and the metabolism of energy and substances in the body.
Now the results are starting to come in.
In the last few years, a number of studies have been published that point to the fact that a lot is out of whack in the body of people with ME/CFS.
Some of the discrepancies have only been shown in small studies and need to be confirmed in larger studies before we can establish whether this is a characteristic of ME/CFS.
Enough results have emerged in some areas that there is reason to believe that some of the findings are characteristic of ME/CFS. They include typical abnormalities in the immune system, cardiovascular system and nervous system.
Problems with the immune system
Several studies suggest that the immune system plays a role.
“A growing body of evidence indicates that ME/CFS is associated with dysregulation of the immune system", according to a review published in 2021.
A review is a survey of previously published research on a topic.
For many people with ME/CFS, symptoms start after an infectious disease like mononucleosis. ME/CFS patients also often have close family members with autoimmune disease.
Researchers have suggested that the activity of the immune system in people with ME/CFS is abnormal in several ways. Some studies, for example, have shown persistent inflammation and increased levels of inflammatory substances such as cytokines. What role they play is not yet clear.
A review from 2019 states that certain cytokines are well documented as being associated with ME/CFS, while another review from the same year did not show any systematic difference in cytokine levels in healthy and sick individuals.
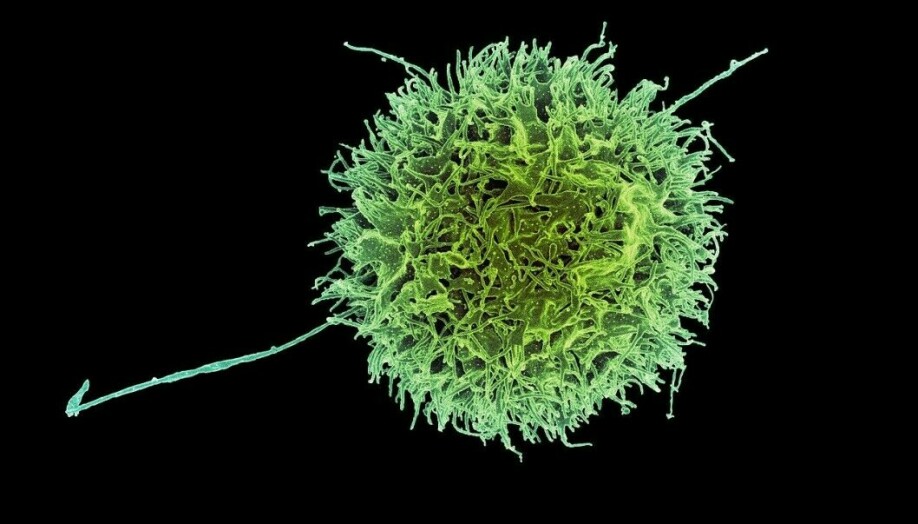
Disorders in immune cells
Other studies have shown disorders in various types of immune cells, such as natural killer cells and T cells. In a systematic review from 2019, the researchers concluded that this seems to be a characteristic feature of ME/CFS patients.
The disease may also have similarities with autoimmune diseases.
“There is compelling evidence that autoimmune mechanisms play a role in ME/CFS,” write the researchers behind a systematic review from 2018.
However, it is not a simple and clear picture, they write. Patient symptoms differ greatly, and the researchers believe that the disease in reality includes several subgroups with different underlying causes.
Autoantibodies and cancer medicine
Research, such as this 2020 review, has shown that some patients have high levels of autoantibodies, which are immune substances that attack the body's own cells. These substances characterize autoimmune diseases.
However, researchers have not succeeded in finding autoantibodies that are specific to all ME/CFS patients. This was confirmed by ME/CFS researcher Øystein Fluge from Haukeland University Hospital at a lecture in 2021. He and his colleagues have been looking for such antibodies for several years without finding them.
Another clue that points to the immune system are experiments with various immunosuppressive drugs, which some studies have suggested may have a positive effect.
A Norwegian study showed that some ME/CFS patients improved significantly after receiving a cancer drug that suppresses cells in the immune system. However, many of the participants experienced no effect, and the results are uncertain since the study lacked a control group.
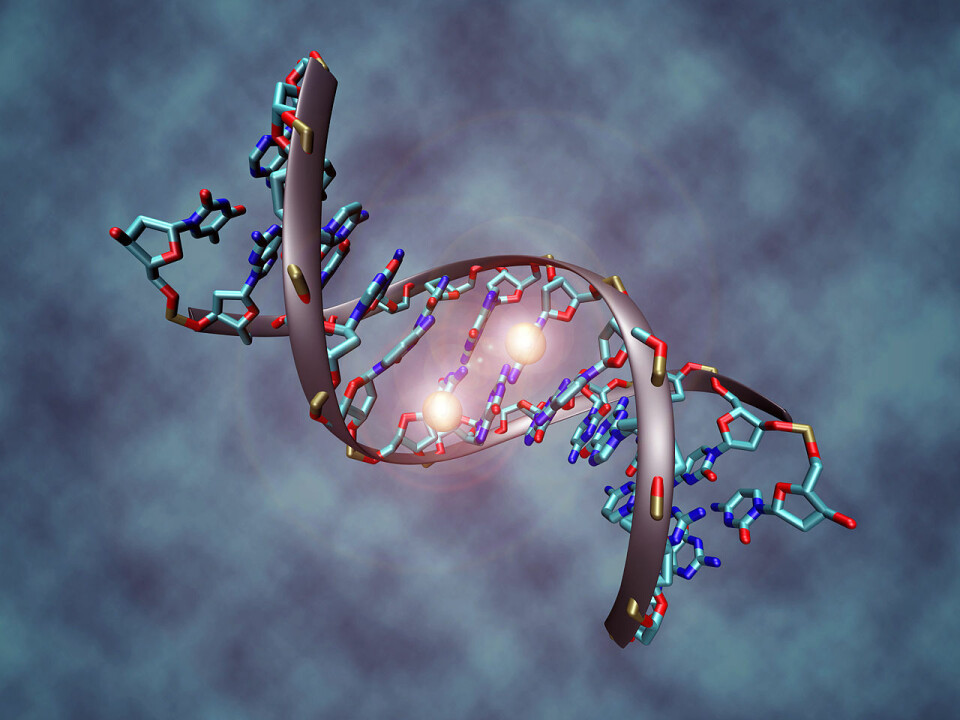
Genes play a part
Other researchers have found traces of the diseases in the genes.
Many diseases are linked to our genes, but it is rare for genes to be the sole cause of an illness. Often people who are affected by a particular disorder have gene variants that make them vulnerable to this specific problem.
Marte Kathrine Viken, from the Department of Medical Genetics and the Department of Immunology and Transfusion Medicine at Oslo University Hospital, looked for recurring gene variants in people with ME/CFS in a study published in the journal Brain, Behavior, and Immunity.
“We see signs that genes controlling the immune system are involved,” says Viken.
These include genes that are linked to autoimmune diseases, where the immune system attacks the body's own tissue.
However, Viken emphasizes that there is no clear and unambiguous connection that explains everything. Finding reliable answers is difficult, partly because these gene variants are quite common in the overall population. Not everyone who has them gets ME/CFS at all.
Genes for immune system and metabolism
Viken's findings reflect other research that has been done on genes and ME/CFS.
Studies, such as this one, have linked ME/CFS to genes involved in the immune system, the hormonal system, metabolism, energy metabolism in cells, and to the regulation of such genes.
Studies like this one have also shown changes in how genes are regulated, known as epigenetic changes.
But each gene is often linked to small effects.
In a review from 2020, the researchers write that ME/CFS is probably due to several factors and that many genes may contribute in different ways. Each individual gene probably has only a small effect, but together they can disrupt several processes in the body.
The authors point out that the studies done so far are small and often not repeated by other researchers. A large systematic study is needed where researchers map the entire genome of thousands of ME/CFS patients.
One such study, Decode ME, is now underway in the UK. Gradually it will be possible to recognize genetic patterns and gene variants that are linked to the immune system or the nervous system.
And not least, metabolism.
Energy trouble
Several studies suggest that the energy metabolism of ME/CFS patients does not function properly, according to the researchers behind a 2021 review of available research.
Studies like this one show disruptions in the processes that convert blood sugar into energy in the cells. The transport of oxygen also appears to be problematic.
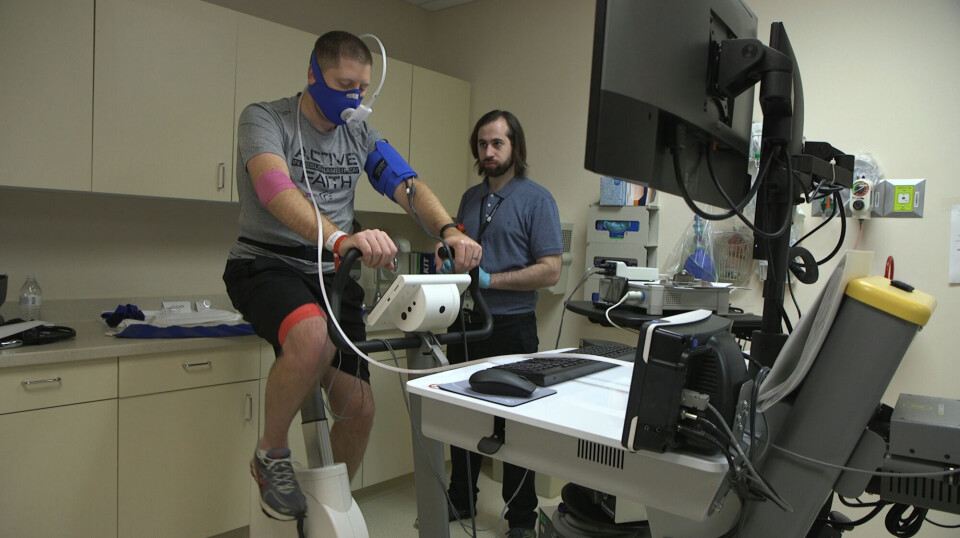
Experiments have shown a characteristic pattern: that the ability of ME/CFS patients to provide energy to the cells deteriorates after physical exertion.
Several researchers, including the Norwegian researchers behind this study in the journal Physiological Reports, have conducted experiments where participants do a physical activity two days in a row.
Normally, both people in good shape and people with poor fitness levels perform equally well on both days. However, the ability of ME/CFS patients to produce energy is significantly reduced on the second day.
This aligns with one of the core ME/CFS symptoms known as post-exertional malaise, also called PEM.
Studies like this one have also shown that ME/CFS patients often have high levels of lactic acid build-up in their muscles, blood and brain, even when they are resting.
The guidelines of the American Mayo Clinic Care Network state that in healthy individuals, lactic acid levels improve with repeated exercise, but this does not happen in ME/CFS patients.
This finding suggests that the people with ME/CFS have problems converting blood sugar into energy. Instead the body switches to anaerobic metabolism, a bit like a normal body does during really hard training.
Changes in the blood
A study from the University of Bergen recently showed that the levels of several substances involved in energy metabolism in the cells were different in ME/CFS patients compared to healthy controls.
“We found changes in 300 different metabolites,” says Karl Johan Tronstad, a professor and one of the researchers behind the study.
These findings may indicate that the cells are struggling to obtain enough energy in ME/CFS patients.
The study results help to gather some loose threads in the research on ME/CFS and metabolism, Tronstad says.
Previous reviews, such as this one and this one, had difficulty in drawing overall conclusions, because the studies that were available were too different in terms of the research methods and which patients were involved.
Another challenge is that it is often not obvious whether changes in the patients are part of the disease mechanism or whether they are due to the fact that ME/CFS patients often tend to be very inactive.
This question is relevant in several areas within ME/CFS research, such as in studies of the importance of intestinal flora.
From IBS to ME/CFS
Linn Skjevling and Rasmus Goll at UiT The Arctic University of Norway in Tromsø fell into ME/CFS research, due to a study on another disease.
It started with the REFIT study in patients with irritable bowel syndrome (IBS).
Previous research has suggested that the intestinal flora may play an important role in this intestinal disorder, and Goll and doctoral research fellow Peter Holger Johnsen tested whether intestinal flora transplanted from healthy people would improve IBS patients’ condition.
“Fatigue is a symptom found in many IBS patients. And the study showed that many of the patients who received active treatment experienced less fatigue,” says Skjevling.
These results led researchers to wonder whether this treatment might also help ME/CFS patients, where fatigue is one of the important symptoms.
Previous research supports the idea.
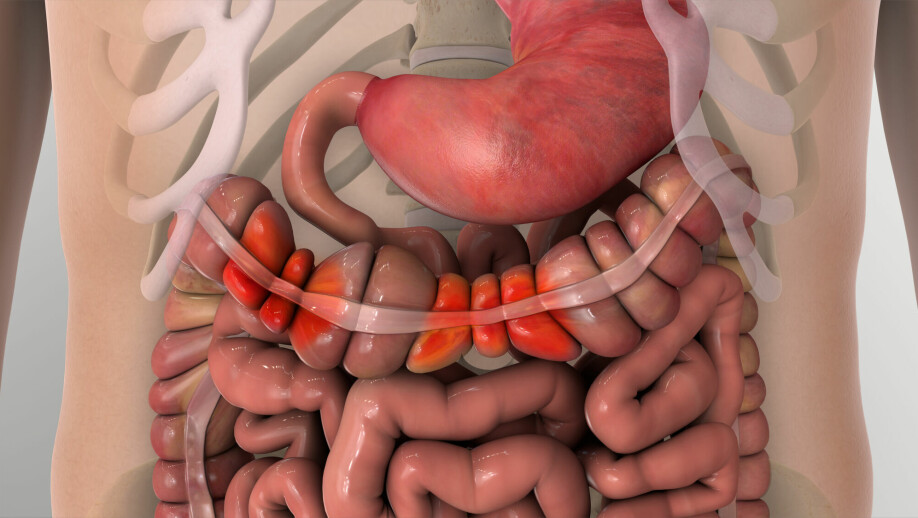
Disorders of the intestinal flora
Many studies suggest that the gut flora could be involved in ME/CFS, researchers concluded in a recent review published in January 2022.
Studies have shown, for example, that many people with ME/CFS have gut flora disorders.
The disorders can in turn be linked to leakage into the intestinal walls and activation of the immune system. The researchers behind the 2022 summary strongly suspect that intestinal flora contributes to creating symptoms in the brain and nervous system.
A lot of research remains, however. An important question that has not yet been well answered, is what precisely leads to what. Do gut disorders lead to ME/CFS, or do ME/CFS and inactivity cause changes in the gut flora?
Skjevling and Goll have plans to dig deeper into these questions.
Intestine could show causes
The Tromsø researchers are now in the middle of a study where they are testing faecal transplantation in ME/CFS patients. It is still too early to say anything about the results. However, if the patients who receive intestinal flora from a healthy donor get better, it would indicate that the gut flora are one of the causes of ME/CFS.
“If ME/CFS itself causes disorders in the intestine, changing the gut flora won’t help,” says Goll.
He and Skjevling are excited about what the results will show.
If the donor flora improves patient health, this might hint at underlying mechanisms that the researchers can study further. And that could in turn pave the way for new treatment.
Goll does not believe that disturbances in the gut flora can explain everything, or that everyone with ME/CFS would benefit from faecal transplantation. But maybe it can help some individuals.
“Even if the treatment only works for 20 or 30 per cent of patients, it’s a good thing, because we don’t have any well-documented treatment right now,” he says.
During the study, the researchers will collect large amounts of data on bacteria, viruses and fungi in the gut, as well as other measures like blood pressure and heart rate which also appear to be disturbed in people with ME/CFS.
Problems in the central nervous system
Several studies have shown that the autonomic nervous system, which controls important functions such as heart rate, respiration and blood pressure, malfunctions in ME/CFS patients.
You can thank this system for allowing you to quickly get up from the couch. The system adjusts your heart rate, tightness in the blood vessel walls and blood pressure, so that the brain receives a steady flow of blood when you stand up.
Several studies have shown that these reflexes do not work normally in many ME/CFS patients. This is according to systematic reviews from 2014 and a more recent one from 2021.
Many ME/CFS patients, for example, experience orthostatic intolerance. This means that they cannot tolerate having their body in an upright position over time – even if they are just lying still, strapped to a table that is being tipped up.
They feel dizzy, and experience symptoms including palpitations, nausea and difficulty thinking clearly.
Tests like these have shown that the pulse and blood pressure of ME/CFS patients do not change as they normally should, significantly reducing blood flow to the brain, according to new ME/CFS guidelines published in the Mayo Clinic Proceedings in 2021.
A study from 2021 which included 199 ME/CFS patients concludes that these differences cannot be explained by ME/CFS patients being in poor condition.
The review mentioned above from 2021 concludes that the available data do not indicate that deconditioning - physiological change following a period of inactivity or a sedentary lifestyle - is the cause of ME/CFS. Nevertheless, poor fitness can aggravate the symptoms, and the researchers call for more research comparing ME/CFS patients with other people having poor fitness.

So many findings – but how are they related?
Although the number of studies on ME/CFS pale compared to other diseases, many measurable differences have nevertheless emerged between ME/CFS patients and healthy individuals.
“I would say that we have so many findings showing differences that it would be difficult to say that this is within a normal range,” says Tronstad.
But the riddle is far from solved.
What does this complex picture of deviations from several of the body's systems mean? How does it all fit together?
What central disease mechanism could explain everything from immune reactions to malfunctions in regulating blood pressure in a standing position?
Vegard Bruun Bratholm Wyller, a professor at the University of Oslo, stands by his statement made to forskning.no in 2018 (link in Norwegian):
“The available research results indicate that this disease is about the interaction of many things. For example, psychological phenomena could just as well explain the biological changes that the patient experiences, as the opposite", he said.
At present, no one knows what disease mechanisms underlie ME/CFS.
But the findings of changes in the body are beginning to point us in certain directions. It seems that abnormalities in the immune system, metabolism and central nervous system are involved.
Several research groups are now trying to piece the findings together into a comprehensive picture.
Blood flow, psyche and immune system
An attempt at an explanation came recently from Bindu D. Paul and his colleagues at the Johns Hopkins University School of Medicine in an article in the Journal of Translational Medicine. They argue that problems with blood flow in the brain can explain many symptoms, such as brain fog, movement problems and sleep disorders.
Several Norwegian researchers have also contributed ideas in recent years.
Emilie F. W. Raanes and Tore C. Stiles at NTNU recently published a hypothesis based on documenting a close interaction between the nervous system and the immune system.
Research shows that the immune system can affect the brain – and, in the opposite direction, the psyche can likewise affect the immune system, they write.
Raanes and Stiles believe that immune disorders play a role in maintaining ME/CFS. They argue that psychological treatment to improve patients’ ability to problem solve, to regulate their emotions and to sleep could help adjust the immune system, which in turn could provide psychological improvement.
It is conceivable that we could tilt the patient towards a positive development in this way, they write.
Disease with two stages
Øystein Fluge, Olav Mella and Karl Johan Tronstad at the University of Bergen have also recently published a possible model for ME/CFS in the Journal of Clinical Investigation.
They believe the findings point to a disease process with several stages.
Fluge and his colleagues think that it all starts with an infection that causes the immune system to react strongly. In this process, both antibodies against the invaders and autoantibodies that attack some of the body's own cells are – most likely naturally – created.
Usually, this reaction subsides once the infection is defeated. But in ME/CFS patients, the researchers believe, something goes wrong.
According to their hypothesis, autoantibodies continue to circulate. They attack and disrupt cells in the blood vessel walls.
Studies, like this one, suggest that people with ME/CFS specifically have a reduced ability to dilate and constrict their blood vessels.
Recently one small study showed that blood from ME/CFS patients actually causes disturbances in cells of the blood vessel wall.
Fluge and colleagues believe that these disturbances cause problems with the blood supply to cells in the brain, muscles and organs. The cells get too little oxygen, which is needed to convert sugar into energy.
Inadequate oxygen might in turn explain many of the characteristic symptoms of ME/CFS, such as fatigue, post-exertional malaise, lactic acid and brain fog, the researchers believe.
But not all of them. This is where stage two comes in.

Body compensates
Failure to convert nutrients into energy in our cells is one of the most dangerous problems the body can have. The body therefore has back-up mechanisms and biological means of dealing with these malfunctions.
“Nothing in the body is as well protected as energy metabolism,” says Tronstad.
If the blood flow is disturbed, the body will try to compensate with secondary adjustments. It can adjust the metabolism and transport of nutrients.
The autonomic nervous system is strongly involved in these compensatory mechanisms. For example, it can increase the heart rate to compensate for decreased oxygen supply.
Fluge and colleagues believe that changes in regulating the autonomic nervous system may cause many of the ME/CFS symptoms, such as problems with digestion and temperature regulation, and orthostatic intolerance, that is, problems with being in an upright position.
Could explain differences in symptoms and treatment effect
The researchers believe that the bodies of ME/CFS patients may use different techniques to compensate, depending on factors like genes, disease severity, level of function, medication, diet and so on. Different people may also have differing abilities to initiate compensatory mechanisms.
“These differences might explain some of the variation between ME/CFS patients when it comes to symptoms and measures that can have a soothing effect,” says Tronstad.
"Some patients might even be in a situation where the underlying autoimmune attack on the blood system is about to stop, but the body still continues its secondary adaptations,” Fluge said at a lecture.
In such cases, measures aimed at the secondary adaptations – such as diet, supplements, careful activity or cognitive support – could have a positive effect.
Just ideas so far
The ideas of the researchers from NTNU and Bergen are captivating.
But many models can seem logical and sensible on paper. Only when the hypotheses are carefully examined do we really get to know what they are worth.
“A hypothesis has to be tested and an attempt made to disprove or confirm it,” Fluge said in the lecture.
“It might be wrong, and then we have to change the hypothesis as new data emerge.”
Judging by the pace of studies in recent years, this is exactly what will happen in the years and decades to come. New studies and better data will give us greater insight into the disease, and hopefully contribute to better ways to treat it.
Difficult diseases are what’s left
Goll from UiT The Arctic University of Norway thinks there is a completely natural explanation for why it is so difficult to get to the bottom of the ME/CFS mystery.
“I think the simple illnesses have already been discovered. Now we’re left with some really complicated diseases that are difficult to understand. They’re ones that may have several triggers and be due to complex systems”, he says.
ME/CFS is far from the only disease we do not yet have a full explanation for.
“Ulcerative colitis is another example. Significantly more money for research has been spent on this than on ME/CFS, but we still don’t know what triggers it,” says Goll.
History has also shown that what we consider to be one disease sometimes turns out to be several. And that even the same disease can have subgroups, with divergent symptoms that benefit from different treatments.
“It isn’t unusual to think that there are subgroups among patients. People with arthritis don’t all have the same gene profile, for example,” says Viken at OUS, who herself has examined the genetics behind several different diseases.
Previous studies of ME/CFS patients, such as trials with the cancer drug cyclophosphamide or cognitive behavioural therapy, suggest that certain treatments may have a big effect for some, but no effect for other patients.
Finding multi-disciplinary explanation
Goll believes that one of the challenges with ME/CFS is precisely that the symptoms span several disciplines.
Thus, the explanation for the disease must also be found across multiple research fields. However, research often does not work that way. Instead, neurologists sit with one bit of the story, cardiologists with another, gastroenterologists with a third, and psychologists with yet another.
It is only when all the parts are seen together that we will have the possibility to understand the whole of the mechanisms involved.
“If we want to end up with a grand unified theory about ME/CFS, specialists from several academic groups will need to come together and connect the dots,” says Goll.
All the researchers sciencenorway.no has spoken to encourage more people to do research on ME/CFS.
“ME/CFS is hugely under-researched. It’s a major societal problem, and it’s completely irresponsible not to try to figure it out. We’ll learn as we go,” says Tronstad.
“I would like to see more research on ME/CFS,” says Viken.
“We have to recognize ME/CFS as a disease that is worth investigating. The more we study it, even on hypotheses that turn out not to be true, the closer we’ll get to an answer as to what is going on”, she says.
Goll concurs, “It’s a good idea to do more research on ME/CFS, both from a humanitarian and a financial standpoint.”
———
Read the Norwegian version of this article at forskning.no
































