The horrific disease that won’t die
The agonising history of leprosy in Norway has been relocated to a museum in Bergen. The misery was so overwhelming that it inspired pioneering initiatives. It resulted in the world’s first patient registry and the discovery of leprosy bacilli.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Registered data from the 1800s is useful for countries that are still coping with leprosy.
While leprosy is a thing of the past in Norway, nearly a quarter million people are infected with the bacteria Mycobacterium leprae annually in poor parts of the world.
Leprosy is referred to as the least contagious of the contagious diseases.
This seems paradoxical from a historical perspective.

The disease was linked to long-term agony, stigmatisation and death.
Myths and fears
Leprosy was clouded by fear-mongering and myths well into the 1800s, when it was a mounting public health problem in Norway.
A lack of effective treatment, dismal housing conditions, malnutrition and poor hygiene all contributed to outbreaks of the disease.

Few treatment methods existed until penicillin and other antibiotics were developed after the Second World War.
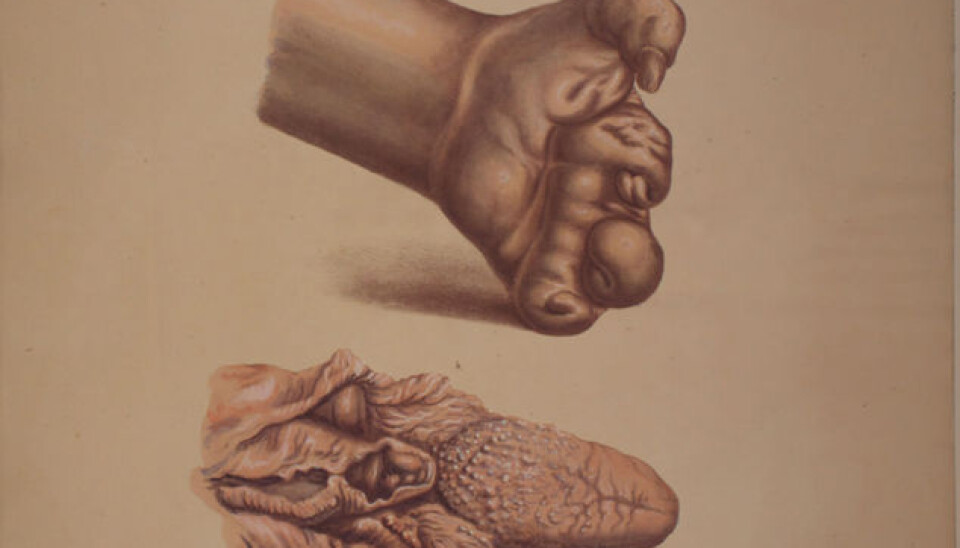
Contracting leprosy was synonymous with an extended death sentence, unless the affliction involved the “knobby”, aggressive form, which played havoc with bodies in a few years.
Patients also faced condemnation and expulsion from the rest of society.
For centuries the malady was considered the work of the devil.
Norway had the highest concentration

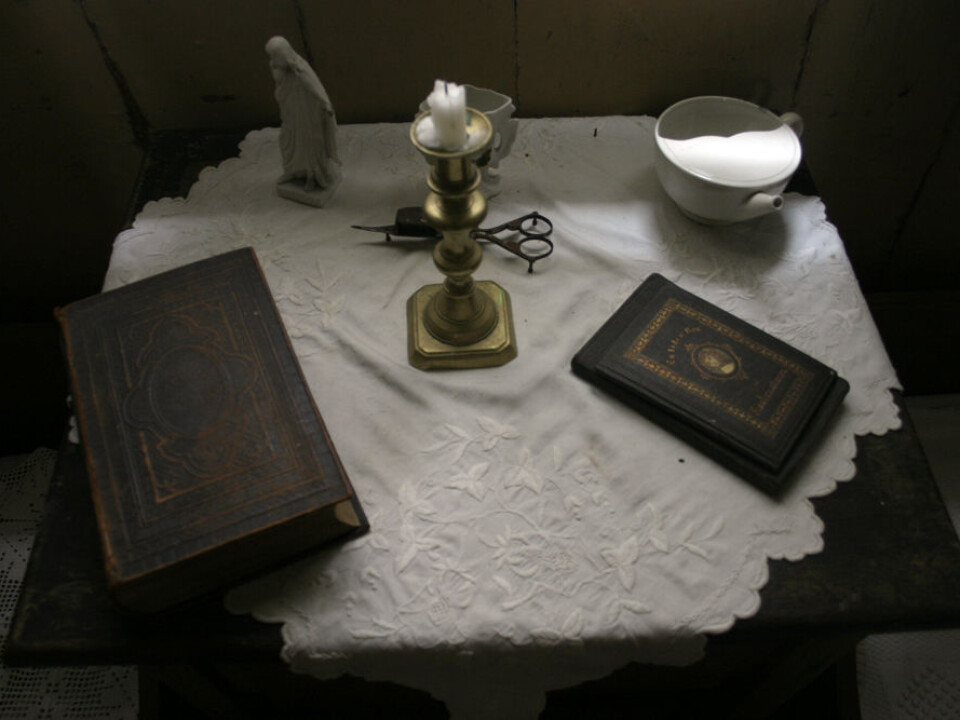
St. Jørgens Hospital in the city Bergen had patients right up until 1946. That was the year the last two died – women, aged 78 and 82.
Leprosy probably came to Europe with the crusades and peaked in the 1200s before finally waning in the 1500s. Except in Norway.
From the mid-1800s until 1900 Norway and Bergen had the highest concentrations of leprosy patients in Europe.
“This led Norwegian authorities and scientists into the most innovative, intense and comprehensive health efforts of the country’s history,” says Grete Eilertsen, a historian and curator at the Leprosy Museum.

Leprosy institutions were established and a national registry was created to record all the cases of the disease. Legislation was passed to deal with isolation of patients as part of the battle against the disease.
Danielssen believed in a hereditary link
The Norwegian Dr Daniel Cornelius Danielssen (1815-1894) ruled the field with his studies for a long time. Along with colleague Carl Wilhelm Boeck he maintained that leprosy was hereditary.
This notion is at the core of the duo’s book on leprosy from 1857.
Danielssen saw that several members of a family could be infected and this led him to believe in a genetic cause.

Hansen’s discovery in 1873
After a while others entered the fray with opposing views, particularly the Norwegian Gerhard Henrik Armauer Hansen (1841-1912).
He encountered a wall of scepticism and resistance from medical circles.
Hansen was educated in microbiology and refused to accept Danielssen’s genetic theory.

“He worked continually according to his hypothesis that leprosy was a contagious disease caused by a microorganism,” says Eilertsen.
Hansen discovered the bacillus in 1873 and a year later he published a description of what he’d seen in the microscope.
He was the first person to show that a chronic disease could be caused by a bacillus, a rod-shaped bacteria.
The scientist was aided in his studies by one the Norwegian authorities’ initiatives.
In 1856 health officials arrived at the bright idea of collecting medical records of all leprosy patients in a single registry.
In fact the Norwegian Leprosy Registry was the world’s first national patient registry.
Why the registry was established
Professor Lorentz Irgens of the University of Bergen says the officials had several reasons for creating this registry.
Irgens revived interest in the nearly forgotten, but rich, leprosy archives in Bergen.
He says physicians and others were clearly concerned about leprosy as a mounting Norwegian public health problem in the latter half of the 19th century. They wanted to prevent further contagion.
They reasoned that the cause of the disease could be discovered by registering all diagnosed cases. A national patient registry would form the basis for contemporary and future epidemiological research.
“Another factor which spurred legislative action was that the disease had spread from the northern and western regions of the country to the east, in other words closer to the capital. This made an impression on the Norwegian Parliament,” explains Irgens.
Completely decisive
The leprosy registry proved to be a key tool in Norwegian public health efforts.
Irgens stresses that the registry was completely decisive in providing Armauer Hansen with the information he needed to report the link to a bacillus.
Hansen also demonstrated how effective the isolation of patients was in warding off further contagion. The Norwegian Parliament passed the so-called leprosy acts a couple of years later in 1877.
After the law was enacted certain poverty relief routines for lepers were ended, according to Irgens. Previously they had been sent from farm to farm to be housed and fed, as part of a social welfare system.
Old registry still useful
Leprosy is considered to be one of the world’s oldest known diseases. For thousands of years it took its toll and unknown millions probably died of it.
Even now an estimated 3,000 persons die of leprosy annually.
The World Health Organization has a goal of wiping out the disease. Despite effective modern atiobiotic treatment, several hundred thousand new cases are diagnosed annually.
Although far fewer patients die now of leprosy, it is still a massive health problem for the victims. They suffer damage to vital organs and their bodies can be deformed.
Norwegian registry findings from the 1800s are still helpful for poor countries that lack such data.
“The results are still relevant. If countries that still have the disease note a high average age among newly diagnosed patients, the disease is declining. The opposite applies if most of the people contracting it are young,” says Irgens.
He thinks the reason why the bacillus hasn’t been defeated is probably that it can survive rather a long time outside a human host. It has other reservoirs.
Irgens explains that leprosy is a problem for the underdeveloped nations because malnutrition leads to a protein deficiency and a generally reduced immune system.
----------------------------
Read this article in Norwegian at forskning.no
Translated by: Glenn Ostling
































