Small additives can make old antibiotics work again
Norwegian researchers have created several promising additives for old antibiotics. But even if they were to reach the market, they would only be a short-term solution. “We can never win the battle against bacteria,” says professor Dag Berild.
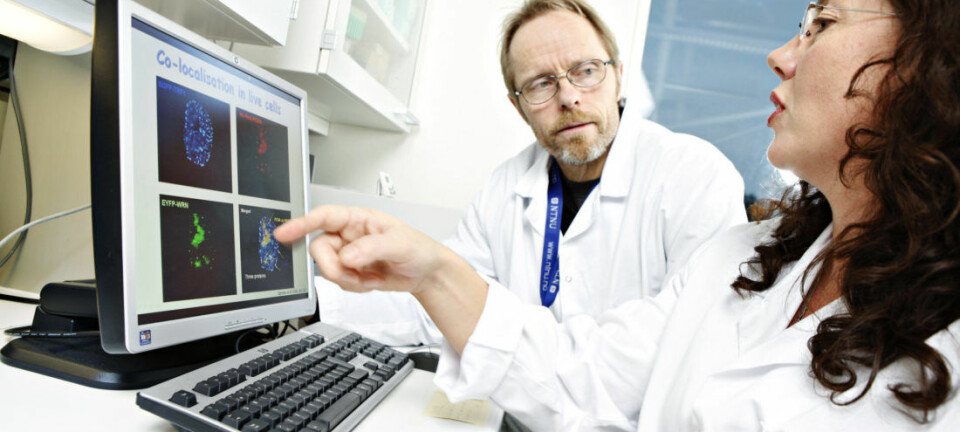
Researchers at a laboratory in Tromsø are testing some very special substances. They are so small that the researchers have to use powerful MRI machines to study them.
On their own, these substances are completely useless in the face of resistant bacteria. Or in the face of any bacteria at all.
They can’t kill bacteria the way antibiotics can.
Nevertheless, they may prove to be important in the fight against antibiotic resistance.
They can make old antibiotics work again.
But to understand how they work, we need to look into how bacteria become resistant to antibiotics in the first place.
Enzymes that destroy antibiotics
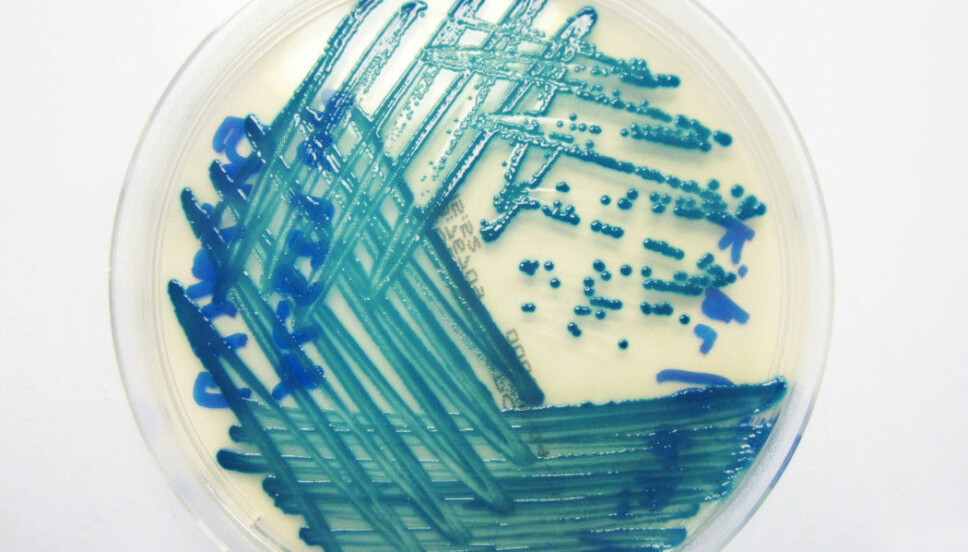
There are many ways for a bacterium to become resistant to antibiotics. But one common feature is that the bacterium can make enzymes that prevent the medicine from working.
Bacteria can easily share these resistance enzymes. This means that bacteria that were previously susceptible to antibiotics can suddenly become resistant. This is a major, and growing problem in the world today.
“If we can’t develop good strategies for treating resistant infections, we can’t do surgeries, administer cancer treatments or allow people to visit the dentist,” says Annette Bayer, a chemist and researcher at UiT — The Arctic University of Norway.
And this is where the additives come in.
The goal is to prevent resistant bacteria from defending themselves against a very important type of antibiotic.
Drugs of last resort
Bayer isn’t studying the normal antibiotic regimen you buy at the pharmacy, but a type of antibiotics of last resort.
These medicines are reserved for patients who have a bacterial infection that makes them very ill — and that doesn’t respond to other types of antibiotics.
This type of antibiotic belongs to a group called beta-lactams, which also contains well-known antibiotics such as penicillin.
“When the antibiotics of last resort don’t work, the patient can die,” Bayer says.
But if some of the small additives being studied at UiT work as they should, they can be given with these kinds of antibiotics.

Exploits a special feature
“These additives we have developed can go into the bacterium and stop the bacteria's defence mechanism. They link to the resistance enzymes that normally stop the antibiotic from working and stop the enzymes themselves from working,” says Bayer.
One of these substances has been given the cryptic name Inhibitor 2b.
This small substance exploits a special property of these bacterial enzymes, which is that they contain the metal zinc.
The resistance enzymes act like small scissors that cut the antibiotic to pieces. And for the scissors to work, the antibiotic must come close to the zinc in the resistance enzymes.
“We’re trying to develop substances that can take advantage of the fact that there is zinc inside the resistance enzyme,” says Bayer.
Puts the bacterial defence out of play
So if one of these additives binds to the zinc, there is no place for the antibiotic and the resistance enzyme is stopped.
“The additives themselves don’t kill the bacterium. The only thing they do is stop the bacterium's defence mechanism from working,” Bayer says.
One of the things that is particularly promising about Inhibitor 2b is that it binds to several different kinds of resistance enzymes, Bayer says.
But there is still a lot of work to be done for either Inhibitor 2b or one of the other additives the researchers have made to be brought to the market.
“The substances work well on the resistance enzymes, but we have to improve the substances' ability to get into the bacteria where the enzymes are found. This is an important focus in our work now,” she said.
And even if they should succeed, it doesn’t mean they have solved the problem of resistance.
Expensive to develop new antibiotics
Dag Berild has been studying antibiotic resistance for years. He is a professor at Oslo Metropolitan University and has worked as a chief physician in infectious medicine at Oslo University Hospital.
He also believes it’s important to develop new additives that can extend the usefulness of antibiotics we already have.
“It’s very difficult and extremely expensive to develop completely new antibiotics. That is why the pharmaceutical industry has abdicated its responsibility for conducting research in this area,” Berild wrote in an email to sciencenorway.no.
He himself has been involved in the work of developing another type of additive called ZN148, which he and colleagues wrote about in an opinion piece in Aftenposten, a Norwegian national newspaper, and on sciencenorway.no.
This drug has also not come on the market yet.
But there are several additives that are already in use. The problem is that they only work against some of the resistance enzymes.
And unfortunately, the additives only work for a short period.
An eternal battle
That’s because when bacteria can no longer defend themselves against the antibiotic, they can develop new resistance mechanisms, Berild says.
This will also be true for Inhibitor 2b and ZN148, if they reach the market.
Consequently, new additives are not the ultimate solution, Bayer said.
“It will still be important to use antibiotics of last resort with caution. We have to reserve them for the most important cases,” says the UiT researcher.
The additives will only make a small contribution in an eternal battle.
“We can never win the battle against bacteria, all antibiotic use leads to resistance,” Berild wrote.
Have to think differently
The most important thing societies can do is to use less antibiotics in the world than are used today, Berild said.
“I think we have to think completely differently in the future, and look at how we can live in better harmony with our bacteria. Our bodies contain roughly two kilos of bacteria, which can be considered a separate organ called the microbiome,” he said.
“The use of antibiotics not only leads to resistance and diarrhoea, but probably also to a number of other diseases. My professor at the University of Copenhagen said more than 40 years ago that antibiotics should be reserved for life-threatening infections, because otherwise things would go wrong. He was probably right,” Berild wrote.
Translated by Nancy Bazilchuk
References:
Z. Muhammad et al.: Structural studies of triazole inhibitors with promising inhibitor effects against antibiotic resistance metallo-β-lactamases, Bioorganic & Medicinal Chemistry 2020, https://doi.org/10.1016/j.bmc.2020.115598
S. Skagseth et al.: Metallo-β-lactamase inhibitors by bioisosteric replacement: Preparation, activity and binding, European Journal of Medicinal Chemistry 2017, https://doi.org/10.1016/j.ejmech.2017.04.035 Summary
———
Read the Norwegian version of this article at forskning.no