
Weak antibiotic doses undermine our body’s defences
Swedish scientists have found how an insufficient treatment can make cholera bacteria resistant to our immune system.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
“Antibiotics are no problem if the dosage is right. But if it isn’t high enough, bacteria counterattack with an alternative strategy,” says Sun Nyunt Wai.
She is a professor at Umeå University in North Sweden. She and her colleagues at the Laboratory for Molecular Infection Medicine Sweden (MIMS) have shown for the first time how treatment with antibiotics develops resistance to our immune system.
Resistant bacteria
Bacteria that evolve a resistance to drugs are nothing new. They reproduce so fast and in such unimaginable numbers that mutations are constantly cropping up that have resistance to antibiotics which were previously effective. The problem is on the rise.
We need to develop new strategies for treating patients. The project at Umeå University links to efforts to understand the molecular mechanisms are making bacteria resistant.
Greater tolerance

The MIMS scientists used cholera bacteria in their experiments. Cholera has killed millions of people and is still a major health problem in certain regions. The bacteria causing the disease, Vibrio cholera, is already highly resistant against antimicrobial peptides. These amino acid compounds are an essential element of our bodies’ immune response.
An array of peptides can work together to fight bacteria. The Swedish findings reveal the risk of the bacterial ability to resist drugs as well as the natural peptides in our bodies.
“The antibiotic drug kills the bacteria. But n sublethal dose of antibiotics enables bacteria to develop a strategy of resistance.”
“We now see that they are not just resistant against a given drug, but they can also withstand the body’s antimicrobial peptides,” says Sun Nyunt Wai.
Protein production
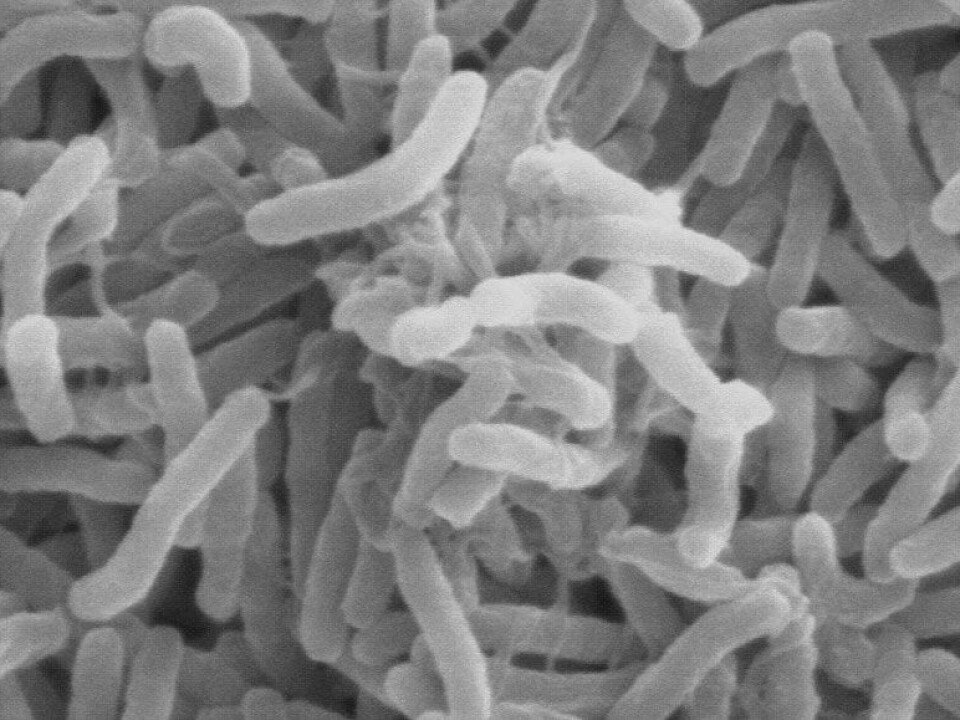
Membrane vesicles are the key to such success – tiny envelopes or sacs on the surface of a bacteria cell.
The vesicles can transport and store various substances. When cholera bacteria grow the vesicles are filled with substances which can impact and damage the human body host cells.
But in this case it turns out they do more than that. When subjected to light doses of an antibiotic called polymyxin, the bacteria formed larger vesicles. They also produced more of a protein known as Bap1.
“We observed that Bap1 binds to structures on the surface of the vesicle and forms molecular traps. These traps are very effective in binding the natural substances the body’s immune system produces against microbes,” explains Sun Nyunt Wai.
“This allows the cholera bacteria to withstand the attacks by deactivating the natural immune response.”
Peptides will normally kill off the bacteria before they do severe damage. But given a non-deadly quantity of polymyxin, the microbes can lock down the peptides and destroy them.
The researchers have carried out the same tests with mutant bacteria which don’t produce the protein Bap1.
“We then saw that the mutated bacteria couldn’t destroy the peptide from our immune system even though they had been given the same doses of polymyxin,” says Sun Nyunt Wai.
She thinks the study clearly demonstrates how important it is to investigate the chances of cross-resistance as a result of antimicrobial drugs.
---------------------
Read the Norwegian version of this article at forskning.no
Translated by: Glenn Ostling


































