Food intolerance is linked to different disorders
Are you convinced you can’t handle dairy products, bread or fruit? Our own perceptions of having a food intolerance appear to link closely to diagnoses such as irritable bowel syndrome, fibromyalgia and chronic fatigue.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
They might seem to be something of a nuisance: the people at your dinner party who claim they can’t eat this or that. They’re always pulling those snap peas out of their salad or scraping the whipped cream off their slice of cake.
Their doctors examine them and find nothing: “No coeliac disease here. Nix on lactose intolerance. Negative on food allergies.”
But Arnold Berstad and colleagues at Oslo’s Lovisenberg Diaconale Hospital think there’s every reason to listen to these patients’ complaints.
The researchers have studied 84 persons who have been referred to gastroenterologists for unexplained digestive problems which the patients themselves think are caused by sensitivity to certain kinds of foods.
Is digestion the cause?
It turned out that all but one of them qualified for a diagnosis of irritable bowel syndrome (IBS). In addition, 85 percent of them had symptoms indicating chronic fatigue syndrome (CFS) and 71 percent showed symptoms of fibromyalgia.
Fibromyalgia is a disorder characterised by chronic tenderness and pains in muscles, tendons and joints. Patients with irritable bowels experience stomach pains and discomfort in the upper stomach region, nausea and often diarrhoea.
Chronic fatigue can cause fevers, swollen lymph nodes, pains in joints and muscles, anxiety attacks, problems with balance, depression, memory and concentration problems and sleep disorders.
The concurrence of all three conditions could point toward a single cause, linked to digestion, writes Berstad and his colleagues in the latest edition of the Scandinavian Journal of Gastroenterology.
They think the significance of the additional disorders suffered by IBS patients is strongly underestimated.
“We were surprised to see how prevalent the other disorders were, and how strong they were too,” says Jørgen Valeur of the Lovisenberg Diaconale Hospital.
No easy tests
One of the biggest challenges regarding patients with IBS, fibromyalgia and CFS is that no simple diagnostic tests are available.
These diagnoses are made on the basis of a pattern of symptoms that cannot be easily registered during a short visit to an MD.
“Many of the patients who are referred to a specialist for their undiagnosed stomach disorders think they are overly sensitive to certain types of food, such as milk, bread or fruit,” says Valeur.
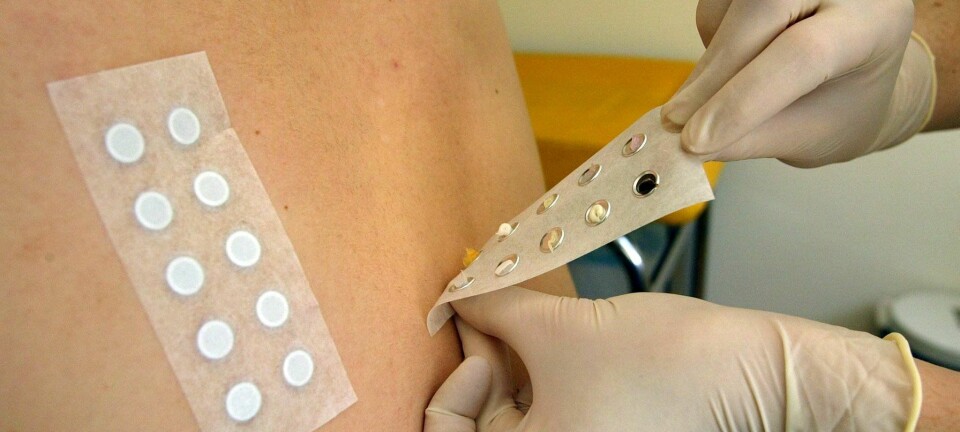
But tests for metal allergies or coeliac disease usually come out negative. The latter is a digestive infirmity that makes patients react to gluten.
On these grounds many doctors have previously disregarded the patients’ claims about having food intolerance.
Recreating stomach problems
“Eventually quite a few give up looking for the cause. There’s a tendency to suspect the problems are psychosomatic, since no physical explanations are evident,” explains Valeur.
“But we’ve had a suspicion that there could be a connection between this self-experienced food intolerance and the triad IBS, fibromyalgia and chronic fatigue.”
The results of the new study could indicate such a correlation. These disorders are not just linked to the patients’ subjective views about having food intolerances.
The stomach disorders can be recreated and observed when the patients are given a synthetic carbohydrate that is hard to digest.
Fine without food
Berstad and his colleagues think it would be unlikely that these patients are wrong about food having an impact on their disorders.
The patients experience that the problems arise in connection with something they’ve eaten. Often their stomachs are fine in the morning or in situations where they avoid food intake. But after meals they feel gassy and uncomfortable.
The problems appear to be linked to intake of carbohydrates that are hard to digest.
“By administering provocation tests in which we give them the non-digestible carbohydrate lactulose we can actually recreate the symptoms that caused them to seek medical help,” says Valeur.
"They don’t get these symptoms if we give them an easily digested carbohydrate like glucose.”
The researchers have also observed an odd phenomenon when the patients eat something they react to.
Get the chills
“Right afterward they get the chills. Their teeth chatter and we have to wrap them in blankets. We wonder if they actually get a fever. We’re investigating that now,” says Valeur.
The medical researchers are also hunting for special compounds from digestion in blood samples from the patients. They think the cause of food intolerance and the three disorders will be found in the intestines.
“We suspect the culprit is intestinal flora. Indigestible carbohydrates, which recreate the patients’ symptoms, are not absorbed in the small intestine but are fermented by microbes in the large intestine,” says the researcher.
He thinks an imbalance in the bacterial flora involved in digestion is disturbing the intestines. This makes the microbes produce substances that create physical problems.
No easy answer
Kirsti Malterud, a professor of general medicine at the University of Bergen, has conducted research on unspecific health problems. She too thinks the three disorders can be linked.
“There are plenty of strong indications of common underlying disease mechanisms for fibromyalgia, chronic fatigue syndrome and irritable bowel,” she says.
“The diseases occur often in the same patient and many of the symptoms overlap.”
But Malterud isn’t convinced that all of this comes from the intestines.
“It’s quite likely that these are severely complex mechanisms involving the interplay of a number of issues,” she says. “Intestinal flora can easily be involved in the disease mechanisms, but it’s doubtful they can provide a single, definitive solution to how these disorders develop.”
Malterud warns that no simple answers can be expected.
“The least fruitful approach is to either claim this is physical or that it’s mental. Of course there’s a connection, also in conditions where there’s no doubt about a role of biomedical mechanisms.”
Remember ulcers
Valeur thinks psychological and physical conditions are involved.
“But we shouldn’t forget the case of stomach ulcers,” he says. “Although stomach ulcer patients displayed a compound array of symptoms, they got well from their physical and psychological infirmities when they got rid of the bacteria Helicobacter pylori.”
“Theoretical models for how psychological and physical factors interconnect could appear informative, but worst case such models can hamper innovative research.”
“Human beings are more than body and soul – we are also intestinal flora,” says Valeur.
Translated by: Glenn Ostling