Treating irritable bowel syndrome with transplanted faeces
Faecal transplantation may work well for some individuals with IBS, a new Norwegian study shows.
More and more studies suggest that the bacteria in our intestines can play an important role in our digestive health, particularly when it comes to irritable bowel syndrome. IBS, as it is commonly called, is a common disorder that causes abdominal pain, bloating and diarrhoea or constipation.
Not surprisingly, this growing understanding of the importance of our bacterial flora suggests that IBS could be treated by manipulating the bacteria in our guts. Or even by replacing it by transplanting intestinal bacteria from a healthy donor.
A limited number of experiments with so-called faecal transplantation support this idea. But overall, there has not been much research on the topic.
A 2017 summary concluded that faecal transplantation needs to be tested by comparing an actual treatment with control groups who are given a placebo, or fake treatment. A March 2018 article written by a team of Norwegian researchers in the scientific journal the Lancet reports on a study where they have done just that.
Donor faeces
Researcher Rasmus Goll and his colleagues examined 87 IBS patients at the University Hospital of North Norway in Harstad.
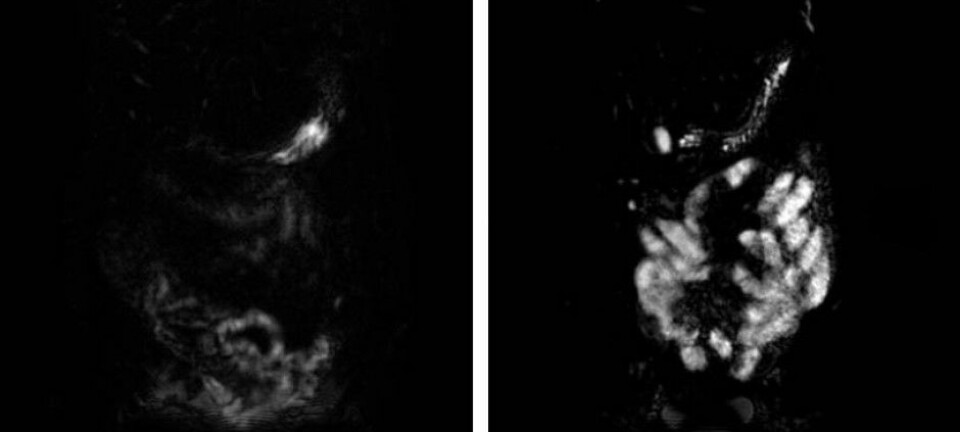
The participants took a laxative to empty their bowels. Then, 55 of patients received implanted faeces from a donor, while the rest instead were given a faecal transplant using their own faeces. The participants did not know who got what.
This approach allowed researchers to see if new intestinal bacteria could help improve IBS symptoms.
Both groups benefitted from the procedure. However, the patients who received donor faeces were doing slightly better than the placebo group after three months. Nevertheless, after one year the effect was gone.
Good and bad news
Not surprisingly, these results are disappointing for those who hoped for a quick cure for IBS.
On the other hand, the study does contain some good news. Goll said the response to the treatment differed from patient to patient.
"Some had very good results while others showed no effect," he said.
The study also found that patients who had other ailments, such as fibromyalgia, chronic fatigue syndrome or depression, often experienced little or no effect beyond the placebo effect. But for those who only had IBS, the situation was different.
"In this group we found a clear, long-lasting effect," says Goll.
He hopes to be able to do a larger study where participants are divided into groups based on their symptoms and any additional illnesses they might have.
It might also be appropriate to give participants several rounds of transplants. It may be, for example, that the new intestinal flora needs several treatments to get established.
On the right track
Arnold Berstad, a professor emeritus and researcher at the Lovisenberg Diakonale Hospital, commends Goll and colleagues for conducting the study. Berstad was not involved with the work.
"These researchers are the first to conduct a placebo controlled study even as the use of IBS faecal transplants has grown worldwide over the last 10 years," he wrote in an email.
Berstad thinks the effects shown by the study are not that impressive. The benefits only lasted for a few months and thus cannot be considered a cure for IBS. Nevertheless, he thinks the study shows this type of treatment has promise.
"I think that this work is on the right track. The next step is to further develop the treatment with regard to curing IBS,” he wrote.
Big difference between patients
Goll believes the differences between patients may be because irritable bowel is not just one disorder. Many who suffer from IBS also have other ailments, which suggests there are different mechanisms underlying the symptoms, he says.
"I think it’s important to take a step back and look at the patients: they are a very heterogeneous group,” he said. “Some people developed IBS after being treated with antibiotics, others after a bowel infection. Some have had the affliction throughout their lives.”
Symptoms of the disorder also differ from person to person. Some have constipation, others diarrhoea. Some have only stomach problems, while others have additional problems such as muscle aches, fatigue or mental ailments like anxiety or depression.
Goll also believes the new results support the idea that we shouldn’t expect to find just one treatment that works for everyone with IBS. Nor should we expect to find a treatment that works both on an individual’s intestinal problems and the additional illnesses that might afflict them.
-------------------------------------
Read the Norwegian version of this article at forskning.no.