Shifting perspectives on Irritable Bowel Syndrome
Irritable bowel syndrome has long been seen as an affliction linked as much to a patient’s mental health as physical health. New evidence suggests the affliction has clear physical causes.
Professor Magdy El-Salhy at the University of Bergen has worked with irritable bowel syndrome for 25 years.
For many of those years, IBS has been considered a somatoform illness—an illness with no clear physical cause, a kind of hypersensitivity with symptoms best handled by a psychologist.
But new research, including El-Salhy’s, suggests that the digestive system of people with IBS does in fact differ from a normal person’s gut in several ways. At the same time, a new treatment that has patients avoid foods with certain proteins, called the FODMAP diet, has brought relief to some afflicted by the illness.
Researchers still do not agree on what causes IBS. But research over the coming years will lead to a better understanding of the disease and improved therapies. Yes, perhaps even ways to cure patients for good.
“I have waited for this a long time,” says Professor Tore Midtvedt from the Karolinska Institutet in Stockholm.
Illness, but no sign of disease
The problem for patients with irritable bowel syndrome is that doctors often cannot find anything wrong. Patients report abdominal pain, gas and diarrhea or constipation. But when they are examined, doctors find nothing.
No sores or changes in the bowel. No reactions to allergy tests. No signs of intolerance.
So it perhaps is not surprising that many professionals have looked to the psyche to find the disorder’s causes— especially because quite a few IBS patients also have psychological problems such as anxiety or depression.
However, new and better research methods have made it possible to look deeper into the body and its cells. These new techniques suggest that there are differences in an IBS patient’s digestive system compared to people without the illness.
Induced IBS in rats
Recently, one study showed that the neurons in the gut of IBS patients appear to be less sensitive than usual. And in 2014, Norwegian researchers found that the intestines of people with IBS actually respond differently to certain substances in food.
Moreover, a great deal of research has shown that people with IBS have a different gut flora than healthy people. It is not easy to determine whether this means that bacteria are helping to cause irritable bowel syndrome, or that irritable bowel syndrome causes the gut to be colonized by different bacteria.
A rat study from 2013 suggests, however, that it may be bacteria that cause IBS, not vice versa. In this study, French researchers reported that they could use bacteria to induce characteristic IBS symptoms in rats.

Previous studies have shown that some IBS patients experience more pain than normal when the intestine is expanded due to gas, for example. Their intestines seem to be more sensitive than normal.
Researchers were able to reproduce this hypersensitivity in rats, just by giving them the microbiota of IBS patients.
Professor Midtvedt at the Karolinska Institutet, who has studied the illness for decades, believes that dysbiosis – an imbalance in the gut flora—is the actual cause of the disorder.
Cured two IBS patients with a variant of the disease
Recently Midtvedt and colleagues reported in a scientific article that they were able to cure two serious IBS cases by replacing the patients’ gut microflora with flora from healthy people.
However, these patients had a variant of the disease, called post-infectious IBS, where their problems emerged in the wake of a stomach infection, or antibiotic treatment. This type of IBS affects less than 20 per cent of patients.
Currently, it is not known whether this type of treatment can also cure people with other types of IBS. But it is not unthinkable.
There are, for example, studies show that the bacterial flora of people with post-infectious IBS is similar to the intestinal flora of other IBS patients.
“We do not know this for sure yet, but I think in principle that there is dysbiosis in everyone who has IBS,” says Midtvedt.
Connecting your gut with your brain
Professor El-Salhy from the University of Bergen agrees that the intestinal flora affects irritable bowel syndrome. But he also says that research has shown that genes, inflammation and diet play important roles too.
And El-Salhy believes we now know how these factors can create the characteristic symptoms that IBS patients experience.
The key, he says, is the neuroendocrine system, an impressive network of nerves and endocrine cells found everywhere in the digestive system. Through the use of hormones and nerve impulses, this system controls everything that happens from the throat to the rectum and more.
The neuroendocrine system can also talk to the rest of the nervous system, including the brain.
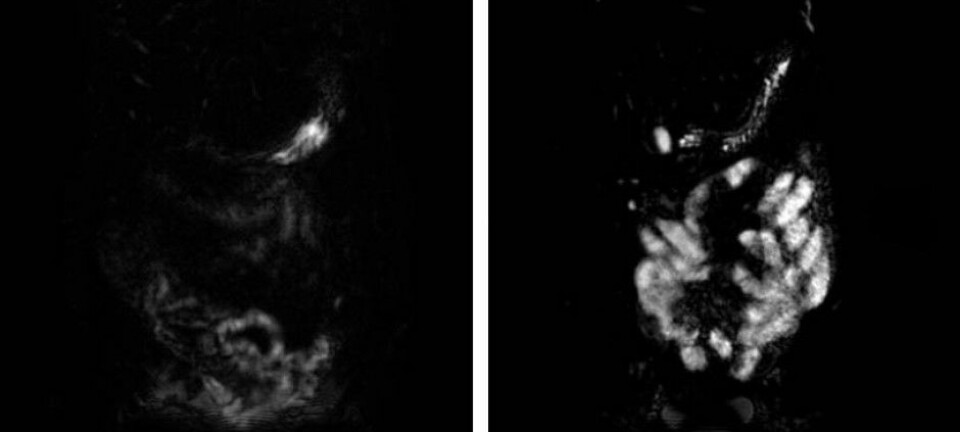
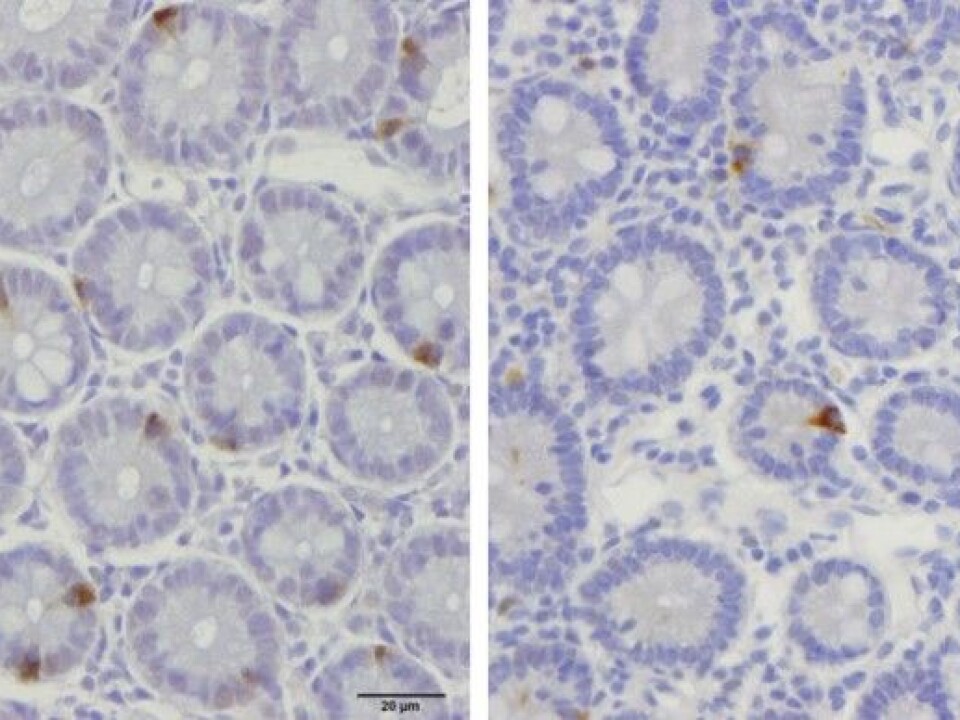
Over the last years, El-Salhy and his colleagues in Bergen have found that people with IBS have fewer endocrine cells in the walls of their intestines and stomach, compared to healthy people.
These results are new, and it will take time and more research before scientists can confirm that irritable bowel syndrome is caused by an incorrect number of endocrine cells. But if this finding holds, it also offers the possibility of a test to confirm that a person has IBS. There is no such test today.
A low FODMAP diet
In 2010, researchers from Monash University in Australia published an article that suggested that people with IBS could reduce their symptoms by cutting out certain types of carbohydrates from their diets. These carbohydrates are called FODMAPS, which stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols.
Today, six years later, the concept and diet are well known among those who either have or treat irritable bowel syndrome.
The research field is still new. But the diet has nevertheless established itself.
But not everyone thinks a low FODMAP diet is a good thing. In 2015 a group of authors in an article in the journal Drugs and Therapeutics Bulletin warned that there is still little evidence supporting the benefits of a low FODMAP Diet.
A few studies have shown that a low FODMAP diet causes intestinal flora to change for the worse, raising the question that we might actually need FODMAPs in our diet to maintain a healthy bacterial flora over time.
On the other hand, El-Salhy and PhD candidate Tarek Mazzawi have found that a low FODMAP diet seems to normalize the number of endocrine cells in the digestive tract of IBS patients.
El-Salhy thinks it’s safe to follow the diet. He argues, however, that many patients can do well by cutting only the most FODMAP-rich foods.
“A low FODMAP diet is complicated and may be difficult to follow for a long time,” he said. “It may be enough to cut out wheat, milk and dairy products containing lactose, along with onions, garlic, beans, peas, artichoke, cabbage, watermelon and artificial sweeteners.”
El-Salhy and his colleagues have recently published several books about IBS and FODMAPs in Norwegian and English, both for professionals and patients.
------------------------------------------------
Read the Norwegian version of this article at forskning.no