A mathematician in the operating room
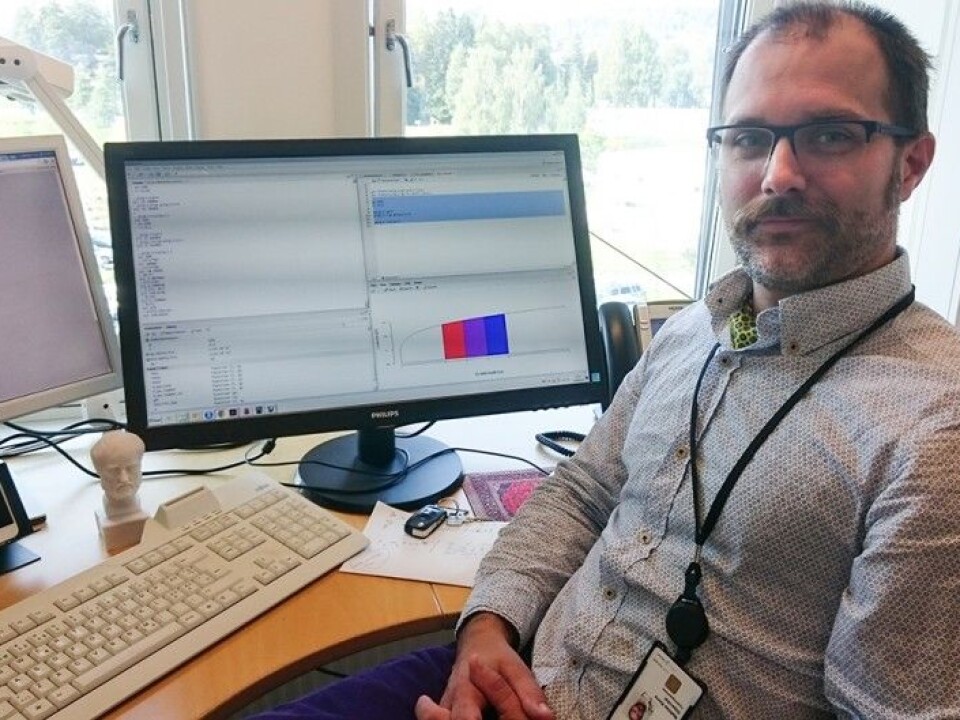
Mathematician Mathias Barra looks at hospitals as if they are health factories. His goal is to find the safest, most efficient way to organize surgery and the use of shared resources.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
In his green gown and face mask, Mathias Barra looks like all the other health personnel crowded around a patient being readied for surgery.
But while Barra hopes his work will lead to better health, he will never place a hand on the patient, nor participate in any operation he observes. His one and only goal is to watch and take notes.
Once the surgery is completed, he’ll enter his data into a computer and try to look for better ways to organize everything using an approach called operational research.
“The goal is to find the answers to the question: How can we perform surgery on as many people as possible, as safely as possible with a limited number of operating rooms and professionals,” Barra said.
Understanding complex systems
Even though Barra is studying medical operations, operational research is not specifically designed for hospitals – or health, for that matter.
Operational research combines mathematical modelling, statistical analysis and mathematical optimization tools to find the best possible solutions to complex decision making problems.
The discipline has its roots in military operations, and in Norway, was used most notably by Kristen Nygaard at the Armed Forces Research Institute in the late 1950s.
Nygaard participated in marches to see observe soldiers’ physical struggles. “Operation Løvsprett” was analysed down to the smallest blister.
Barra has followed the same strategy. He has spent time with surgeons and other hospital professionals from when they first wash their hands to when they sew their last stitch. He has measured the time it takes for each task and mapped out who is doing what - and when.
Introducing the erratic
Barra is trying to build a mathematical model that sets up rules for how actions in the operating theatre unfold.
His computer models are not deterministic. They are stochastic, meaning that they introduce randomness into the mix.
This is how Barra and other mathematicians simulate reality, which is often unpredictable. It’s an approach that follows in the footsteps of Kristen Nygaard, who with his colleague Ole-Johan Dahl developed a programming language, Simula, in the 1960s, which was capable of performing simulations.
Many small steps

As it happens, Ole Johan Dahl's son Fredrik Dahl leads the group for operational research where Barra works. The world is small – and complex.
“Ideally, we would like to do experiments with the model in several alternate realities in the operating room. But we cannot,” says Barra.
Operational analysts have to be content with studying the reality that actually unfolds with the first cut of the scalpel.
“So we need to adapt the model so that it matches better and better with what we actually see. It is a gradual process,” says Barra.
Answering “what if …” questions
Once the model is good enough, it can be used to simulate other ways of running the surgical suite.
It can answer questions such as: What if we bring on an additional doctor?
Or: What if we offset two operations in time so that a shared resource – an anaesthesiologist – has time to go from one operation room to the other?
Another example: Some types of operations vary widely in the amount of time they require. Others are more routine and predictable.
“We can schedule operations that take predictable amounts of time more closely together in the computer program and spread out those with large variations in the amount of time they take,” Barr says. “That way we spread the uncertainty around and it is less likely that there will be a series of delays.”
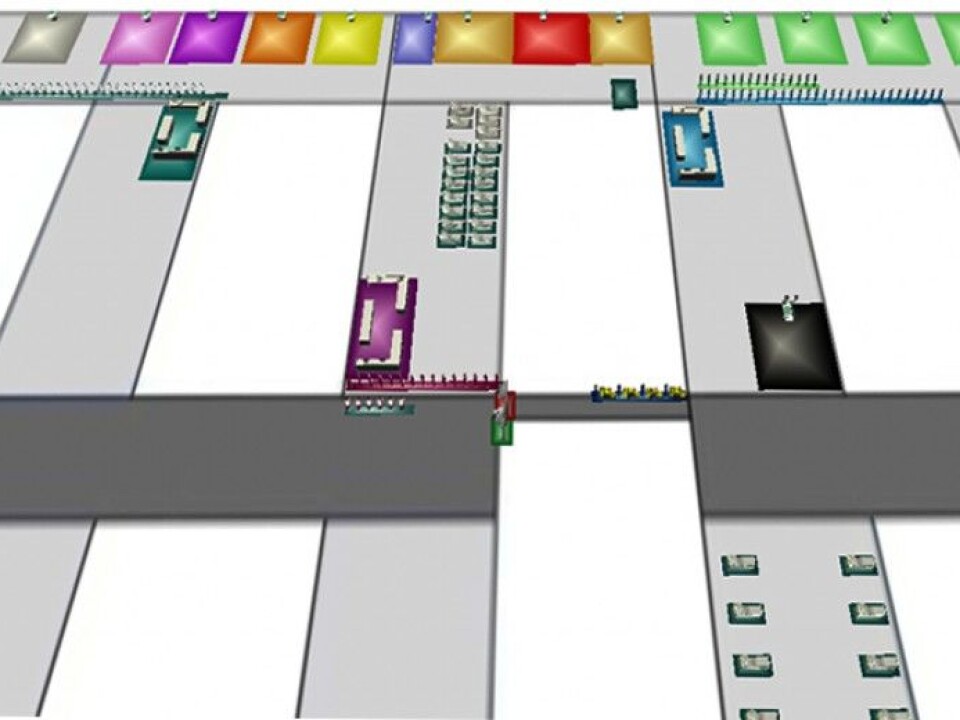
Animated surgeons, patient flow
When he and his colleagues want to suggest changes in procedures, they need to visualize what they mean for the doctors and nurses who actually perform the operations. It simply won’t work to go down to the doctors and nurses with printouts of computer code.
“We use programs that can animate simulations. They look almost like computer games, and show a virtual operating theatre where there are animated computer characters moving around,” says Barra.
Operations are not the only health service that Barra can analyse. Operational research has also been used to study what is called patient flow.
“How can you best schedule patients for shared resources such as MRI scanners and beds? How can as many stroke patients as possible be helped through therapy and rehabilitation?” Barra says. “Without this kind of analysis, there might be even more patients in hospital corridors than we see today.”
Health factories
In spite of the nursing care and the meetings between people, a hospital is also like a factory. It’s like big, complicated machinery, says Barra.
But Barra is careful to emphasize that he does not see himself as a money saver.
“The amount of money that is allocated to health services is a political issue. What we are doing is to help get the most and best possible services out of every health kroner,” he says.
-------------------------------------
Read the Norwegian version of this article at forskning.no