
An artificial pancreas is in the works
People with type 1 diabetes rely on insulin injections or pumps to survive. Norwegian researchers are racing to create an artificial pancreas that would revolutionize the way this disease is treated.
A nearly 2,7 million euro grant from the Research Council of Norway could go a long way to completely change the way people with type 1 diabetes live, if the recipients, researchers from the Norwegian University of Science and Technology (NTNU), are successful. The goal of the research group is nothing less than to create a fully operational artificial pancreas.
“The aim of the project is for people to almost forget they have type 1 diabetes,” says Sven Magnus Carlsen, an endocrinologist and leader of the group.
Carlsen’s research team also includes cybernetics experts, who work with feedback loops and operations in machines, like robots, and in living systems.
The idea to design an artificial pancreas is not unique. A number of other research groups worldwide have the same goal, especially with the approach of 2022, which marks the 100th anniversary of the first use of insulin in diabetics.

But the researchers at NTNU and St. Olavs Hospital in Trondheim believe they have an ace up their sleeve. They are pursuing a completely different approach than other research groups.
Insulin delivery, via pumps or needles
Type 1 diabetes occurs when the pancreas does not produce insulin, which the body uses to regulate sugar levels in the blood. Nevertheless, most people with type 1 diabetes can lead normal lives, as long as they are careful. They have to eat a healthy diet, exercise, and monitor their blood sugar levels, so that they can supply their bodies with insulin via a syringe or a pump.
Insulin pumps provide regular doses of insulin throughout the day, while injections of insulin are calibrated by patients according to what they have eaten or how much exercise they have had.
When the pancreas functions as it should, the human body regulates blood sugar levels flawlessly. Patients, on the other hand, may not be as successful. This can pose short-term problems, but the biggest problem is that poorly controlled blood sugar levels can cause serious damage to the body over time, including heart, kidney and eye disease.

An artificial pancreas would act just like a flesh-and-blood pancreas, by measuring blood sugar continuously, calculating how much insulin the body needs at any one time, and then dispensing the insulin automatically.
Time lag with low blood sugar
Producing an artificial pancreas may sound like a simple task, but it is not. The system has to measure glucose levels in painstaking detail and in real time. In addition, it has to deliver insulin that will act as quickly as possible. The goal is to keep your blood sugar from getting too high—or too low.
The biggest challenge is measuring blood glucose levels in real time without having to take blood samples several times during the day.
In other, similar efforts to create an artificial pancreas, researchers have adapted ready-made blood sugar monitors that are implanted just under the skin to measure blood sugar levels. The meter is connected to a small computer, which transmits the measurements to a conventional insulin pump. The pump then injects insulin into the body.

But the NTNU research group does not think this is the solution.
“It can take a good 15 to 20 minutes from when blood sugar reaches a certain level until the meter picks up the change,” says Carlsen.
“But the greatest time lag is from when insulin is injected into the body. Even if you use fast-acting insulin, it doesn’t take effect until about an hour after it is injected into the body. It would be as if you were driving a car and turned the steering wheel, but the car didn’t respond until a few hours later,” Carlsen said.
Other researchers have also been critical of this lag in the system.
In the worst case, the time lag can cause dangerous complications. If the patient gets too much insulin, he or she risks having seriously low blood sugar. This can result in difficulty speaking, double vision, coma and even death.
An opening in the stomach
Carlsen and his colleagues plan a system that will overcome these problems by measuring glucose in the abdominal cavity. They will do this by monitoring glucose levels in the peritoneal fluid, which is the fluid that covers the surface of the intestines. They will also administer insulin into the peritoneal fluid. Research from both the NTNU group and others suggests that this will make measurements more precise, and that insulin will be absorbed much more quickly if it is injected directly into the abdominal cavity.
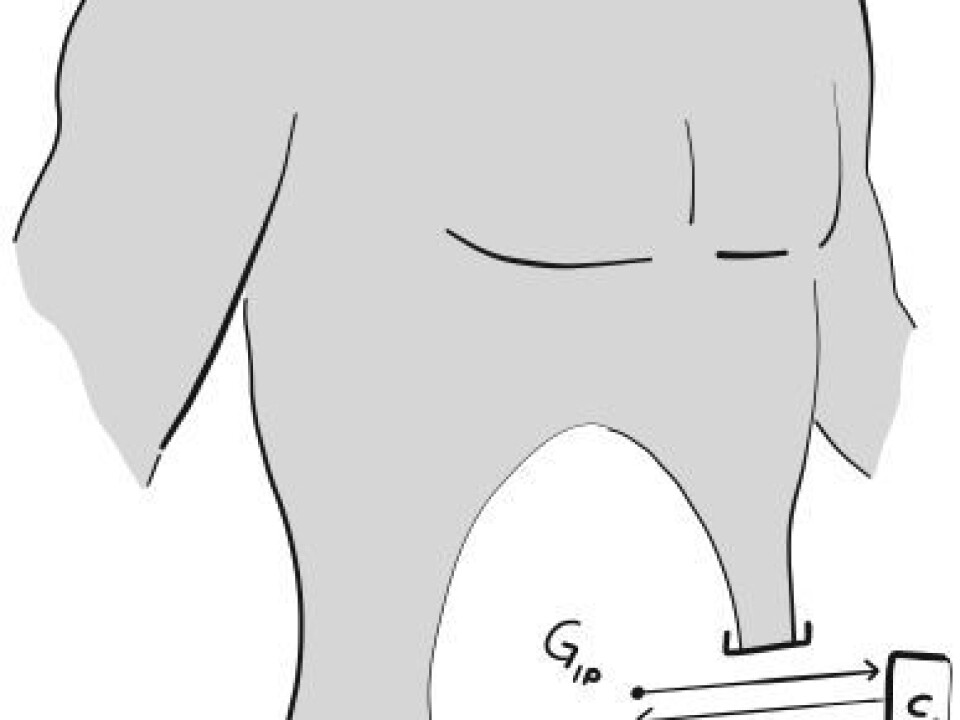
The researchers will surgically open a small hole in the abdominal wall, through which they will insert a thin tube with a sensor on the end. The other end of the tube will remain outside the body, where it will be connected to a small glucose meter, an insulin pump and computer, all in one.
The machine will be the size of a smart phone and will determine how much insulin the body needs. The opening into the stomach will be about one-half to one centimetre in size. The tube will be about the diameter of thick twine.
It will also be possible to remove the system for short periods, such as in the shower.
Fill it and change the battery
“The only thing the user will have to deal with is refilling the machine with insulin and replacing the battery,” says Carlsen.
Another research group based at Harvard University has been working with an artificial pancreas that measures glucose levels under the skin.
The leader of the project, Frank Doyle, wrote to ScienceNordic’s sister publication, forskning.no, that his group agrees with Carlsen that measuring glucose in the abdominal cavity is the best solution.
“But this method is still at the beginning stages,” Doyle wrote. And while he agrees the preliminary results are promising, he also points out that the method also requires more invasive surgery.
------------------------------------------------
Read the Norwegian version of this article at forskning.no


































