Norwegian researchers want to make a universal vaccine covering all coronaviruses
It is possible to make a universal vaccine against the flu virus – one that would give broad protection against all the mutations this virus is famous for. Norwegian researchers are now exploring whether the same method can be used for the coronaviruses.
Bjarne Bogen doesn’t really want to talk about it.
For years, his focus has been to create a universal vaccine against the flu virus – that is, a one-shot-vaccine that would protect you from all the different strains of the flu virus – those we know of, and those that may come.
And this is still the main focus, the universal flu vaccine, which has shown great promise. On March 6th, Gunnveig Grødeland, a researcher who is collaborating with Bogen on developing the vaccine, stated in newspaper Morgenbladet that they were not interested in going after this new coronavirus.
But a few weeks ago, Bogen ordered genetic sequences of the coronavirus.
And so come the beginning of April, and Morgenbladet could tell their readers that Norwegian researchers are now joining in the efforts to create a vaccine against Covid-19.
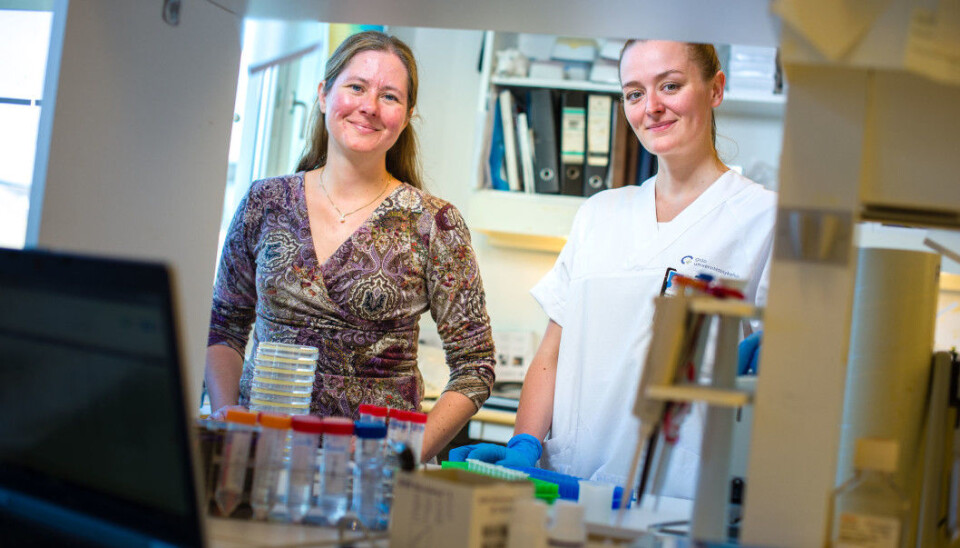
“We haven’t changed our course”, insists professor Bogen, who is the group leader of the team Cellular and Molecular Immunology at Oslo University Hospital.
And the goal is not to ‘win the race’ – this wouldn’t be possible given what it is Bogen and his team are trying to achieve.
“People have already started clinical trials in humans. We’re about to test some simple things in mice. We’re not competing”, he says.
But if they eventually succeed, their vaccine will be the best.
A molecule makes all the difference
The idea then is to take the work they have done on the flu virus and apply this to the coronavirus.
The key to a universal flu vaccine lies in the surface of the viruses, according to Bogen. This is where we find the proteins, spikes on the surfaces of the virus that our immune system can recognize. The most important of these on the flu virus are the proteins called hemagglutinin. Instead of injecting whole or large parts of the virus into the body, Bogen’s method is to focus on hemagglutinin.
“Our vaccine codes for protein, and it’s the protein which gives the immune response”, says Bogen.
The coded proteins are encoded by a DNA plasmid and shot onto naked skin using compressed air.
Bogen’s team is not alone in this world in trying to create a universal flu vaccine. But they do believe they have something unique to offer: a patented molecule which acts as a targeting unit in the vaccine, ensuring that the bits of the virus in the vaccine are directed toward the most relevant immune cells.
“Because of the way the viruses have developed previously, we know that some parts of the surface proteins don’t change as much as the others. And if you can generate immune responses against these areas, you win. To simplify, we try to remove that which is different and increase the concentraton of that which is common. And because we use this targeted method, the immune response is all the more powerful”, explains fellow Ane Marie Anderson from Bogen’s lab, to Morgenbladet.
It’s working well in mice
In a first test on mice, a broad flu vaccine using this technology contained the recipe for seven variants of hemagglutinin, so seven different types of flu viruses.
“Upon vaccinating the mice, we observed substantial immune responses towards all the influenza types covered by the vaccine”, said Grødeland in an article on the University of Oslo webpages. The mice even gave protection against viruses not included in the vaccine.
Grødeland worked on Bogen’s team until about a year ago, but is now group leader of her own team, under the name Influenza and adaptive immunity. The vaccines in question are now a joint effort of Grødeland and Bogens groups.
“By using DNA it’s easy to include components from several different viruses”, says Bogen.
“And this in turn gives a much broader immune response covering all the viruses”.
The next test in mice included 18 variants of hemagglutinin, from the 18 known sub variants of the flu virus.
The results from this study have not yet been published, but Grødeland and Bogen can reveal that it went very well. Any more details will have to wait until after peer review. And then of course remain the clinical trials to test this in humans.
Enter the coronavirus
“Just as with the flu, we’re thinking that if you can take different elements from different coronaviruses – perhaps even those you find in bats and that haven’t yet appeared in humans, then we can make a broad vaccine which will give a broad immune response that works against all these different strains”, says Bogen.
And this type of broad corona vaccine will likely be necessary. SARS-CoV-2 is not the first coronavirus to hit human beings, and it probably won’t be the last.
“We had SARS in 2003, then MERS in 2012. Now there’s COVID-19 in 2019. All of them coronaviruses that jump from bats to humans, or camels in the case of MERS. We cannot be certain that this is the last time this will happen. And we can only speculate about whether this has happened previously in history, before we knew what viruses were”, says Bogen.
We can’t know what the next coronavirus will look like, but it will most likely be similar to the viruses that cause SARS and COVID-19, according to the professor.
“Many of the viruses you find in bats are similar to these two viruses”, says Bogen.
But before the team can fully apply their technology to the coronavirus, they need to know more about how it interacts with our immune system.
“An important part of the puzzle is to find out which type of immune response that gives the best protection against the coronavirus”, says Grødeland.
“More research is needed before we can identify this. Our main goal is always to learn more about immunity, so we can create even better vaccine strategies. We’ve started making some vaccines for the coronavirus now, and will use these to study what kind of immune response that gives protection”, she says.

A durable DNA vaccine
Two of the more famous attempts at making coronavirus-vaccines at the moment are the one from American biotech company Moderna (who are already testing in humans), and the German biopharmaceutical company Curevac (the one Trump allegedly wanted to buy). Both of these vaccines are based on RNA – a family of molecules that are similar to DNA, but whose function is slightly different.
“If the genes (DNA) are the encyclopedia, then mRNA is more like the hand-written notes that you make when you need to go shopping”, writes researcher Sven Even Borgos in an opinion piece on the development of new RNA-vaccines for the coronavirus. DNA is durable. RNA is more fleeting.
“RNA has become very popular to use in vaccines”, says Bogen.
“It can have some advantages, depending on your perspective and who your vaccine is for”, he says.
A worry when using DNA in vaccines, is that this foreign DNA may infiltrate the host DNA.
A Norwegian company that uses DNA in its vaccines is Vaccibody. The technology used in this company’s tailor-made cancer vaccines was developed in Bjarne Bogen’s laboratory between 2002-2007 and is based on the same sort of technology involved in the work on the universal flu vaccine.
“When you’re using DNA in a cancer vaccine you don’t have to be so worried”, says Bogen.
“These are patients who often have poor prognosis. If you can cure them then that is such a massive achievement, that you don’t worry so much about the DNA in the vaccine potentially integrating into the recipient DNA.”
If however the DNA vaccine is intended for, well, the entire world population, then this becomes more of an issue. In any case, most research indicates that this risk is not very high, according to Bogen.
RNA has an advantage over DNA when it comes to this worry. RNA is degraded – so you are guaranteed that it won’t integrate.
DNA also has its advantages, for instance that it is tougher and thus can handle rougher treatment. And it takes a long time to degrade.
“Today for instance, we can still isolate DNA from Neanderthals. DNA is a lot more durable than RNA. RNA actually has to be reshaped in vaccines to make it more resilient”, explains Bogen.
DNA vaccines are also easier to make in large quantities and are easier to transport as they don’t have to be kept cool, both qualities that perhaps make DNA-vaccines particularly apt in responding to pandemics.
Science takes time
Bogen is not a fan of talking about research before it has been peer reviewed and published.
“What I can say is that the principles for this method which we published in 2018 still hold, after we have done more comprehensive and extended studies. But these results have not yet been published”, he cautions.
“I still want to stress that we don’t really have anything to tell you yet, we’ve barely even started. But we are thinking about it because we’ve had some success with influenza”, he says.
“It is possible to make a universal vaccine against the flu. So now we wonder if we can do the same with the coronaviruses.”
But it will take time.
“I think perhaps five years is a best-case scenario”, says Grødeland.
“But then again you never know. Things can change all of a sudden if what you create ends up being a really good vaccine”.

































