
Norwegian health official: "We don’t think it's possible to stop the COVID-19 epidemic"
Will the coronavirus disappear from Norway after weeks or months of social isolation? Not at all. In all likelihood, there will be more sick and infected people than ever. We have asked Geir Bukholm from the Norwegian Institute of Public Health about what the plan for Norway actually is.
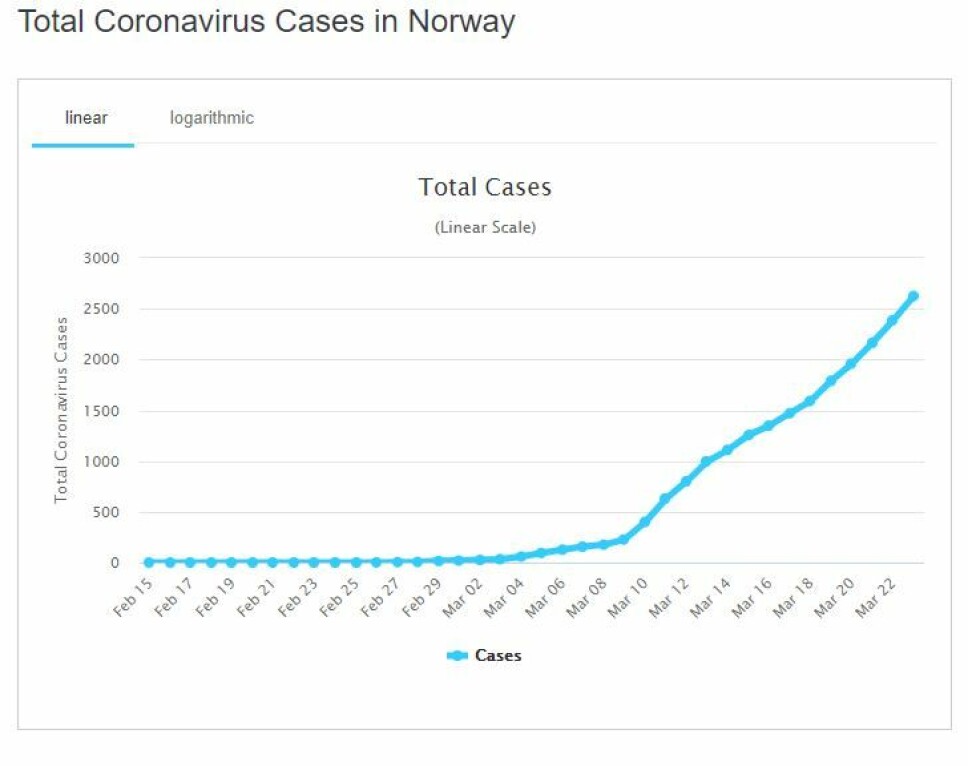
On March 12th, Norway officially shut down large parts of society in order to curbe the spread of the coronavirus. Schools and kindergardens were closed and Norwegians were told to work from home if they could. More measures followed in the coming days, and there are more to come.
Well into the second week of social distancing, closing borders, shut downs and financial crisis, many Norwegians eagerly await the flattening and downard turn of the coronavirus infection curve.
They are in for an unpleasant surprise:
“We don’t think it is possible to stop the epidemic,” says Geir Bukholm, executive director of the Norwegian Institute of Public Health’s Division of Infection Control and Environmental Health.
Over the next year, the total number of infected people in Norway is likely to rise to over two million.
“Our latest estimates suggest that 40 to 60 per cent of the Norwegian population can be infected,” says Bukholm.
Trying to control the rate of the increase
The purpose of the measures that the Norwegian government has instituted to date is to make the increase from a few thousand to millions as smooth as possible.
“We are trying to allow for a controlled epidemic in Norway, one that happens so slowly that we are able to maintain our health care capacity for people with the coronavirus, but also for other patients in need of urgent care,” he says.
“We are also evaluating whether we can delay the epidemic, so that medicines and vaccines that are under development can have an effect for those who may or may have a complicated course of disease. Eventually, the epidemic will burn out,” he says.
By this last, Bukholm means that so many people in the population will have become immune to the disease that it is no longer able to spread.
But how will Norwegian health authorities bring about this controlled epidemic?
Avoiding yo-yo measures
Many people may have thought that the strict measures now in place will significantly reduce the number of infected people, so that the different restrictions can gradually be eased up. At least until the epidemic possibly flares up again and people have to begin a new round of social distancing and isolation.
But that’s not what the Norwegian Institute of Public Health Institute is thinking.
Bukholm emphasizes that it is ultimately politicians who decide what measures to take.
But from an infection prevention standpoint, he envisages that the strong measures that are currently in place in Norway, with widespread closures of schools and the like, will last for a few months to come. At that time, the Norwegian Institute of Public Health will probably recommend that these measures be eased, little by little.
Not because there are fewer infected people, but because there are more.
Some measures won’t work well when infection levels are high
“As the proportion of infected people reaches a certain level, some of the efforts we’ve set into motion will no longer have an effect. Like quarantine measures, or testing people with mild symptoms,” says Bukholm.
“We will continue to see a benefit of measures that limit contact between people, but this effect will also become weaker as we reach a saturation point,” he says.
Bukholm also believes that schools and kindergartens can be opened eventually, both because children seem to contribute little to spreading the infection and because it is going to be very important that the most number of parents be able to work when many in the community will be unable to work because they are sick.
Bukholm expects the epidemic to continue for much of 2020. During this time, both the population and the health care system will be under pressure. But the situation is likely to turn out very differently for different people.
On the positive side, more than half of those infected will hardly notice that they are ill.
On the negative side, the disease can take many lives and mean that people in risk groups will have to remain isolated for a long time.
Enormous range of symptoms
Bukholm said it’s quite difficult right now to say how many people are at risk of dying, in part because of one of COVID-19’s characteristics: The enormous range of symptoms.
At one end, many people can be infected without a single symptom, and many who will feel as if they have a slight cold. At the other end, people will succumb to double pneumonia and organ failure.
This range separates the new coronavirus from other epidemics, such as SARS and MERS. It is also one of the reasons why the new coronavirus has spread across the globe at record speed.
Of course, it’s a good thing that most people who get infected will have a relatively mild case. But at the same time, that makes it extremely difficult to get an overview of how many people are actually infected. This fact also has a lot to say about the possibility of stopping the epidemic.
Probably many asymptomatic cases
Many infected people probably do not even suspect that they are carrying the disease, which means they can be spreading the virus unknowingly.
Bukholm believes that the number of infected people in the Norwegian population is far higher than the number of recorded cases. The Norwegian Institute of Public Health has now developed models that will calculate the actual number of infected people from day to day.
Epidemiologists need to know this number to be able to predict how many people will die during the epidemic. The actual mortality rate will be far lower than 2 to 3 per cent, as can now be seen from statistics from several countries.
The real figure is probably just under one per cent, Bukholm believes.
But even with this mortality rate, many thousands of people will die if half the population is infected. Especially if the disease affects a higher percentage of people in risk groups.
Difficult for people at risk
“We want to skew the infection, so that the people who are not infected are people in the risk groups,” says Bukholm.
But it's not going to be easy. It may be possible to take action at institutions where people are cared for, such as old age homes, and other places where there tend to be many people in risk groups.
But many people who have diabetes, lung disease or are on immunosuppressive drugs — all of which put them in a risk group — are spread throughout the population.
The future ahead for these people can be very difficult, as more and more people in society become infected.
These individuals should probably continue to have limited contact with other people in the community, says Bukholm.
May want to test for immunity
Eventually, many people will also become immune, so that they can safely mingle with sick people. They will also be able to be with people in the risk groups, without the risk of infecting them.
But one challenge is that most people cannot be sure if they have had the disease. After all, many people will have gotten COVID-19 without noticing a single symptom.
“It may be appropriate to start testing people gradually,” says Bukholm.
This requires a different type of test than what is being used to detect the illness today. Instead of testing to see if the virus is in the body, it will test for antibodies in the blood, which show that the body has at one time or another been infected by the virus.
“This kind of test for the coronavirus has not been used for routine testing yet, but they are working to develop them for routine use,” says Bukholm.
Here, we’re more or less making it up as we go.
Don't know if having the disease provides immunity
As we gain more knowledge, both measures and projections for the future are likely to change.
There is still a lot we don’t know. One very basic thing that remains unclear is whether the coronavirus will eventually disappear, or whether it will continue to circulate through populations worldwide, as some other coronaviruses do.
We also don’t know for sure that people who have had COVID-19 actually become immune to it. And how long that immunity possibly lasts. This will also affect the ability to make a vaccine.
Bukholm is nevertheless optimistic about vaccines.
“There are several good vaccine candidates, and I think we will succeed in making a vaccine,” he says.
In the long term, vaccines will become an important tool in protecting vulnerable groups that have not had the disease.
A dress rehearsal
So everything suggests that 2020 will be a different, tough year for most, and for some, a very difficult time. But Bukholm thinks one positive result could come from the ordeal.
This is, in a way, the big test of how humankind copes with a pandemic, a test which thankfully has a relatively low mortality rate compared to diseases like SARS and MERS. This may mean that we are better equipped to deal with a future pandemic of a much more serious nature.
“Yes, this is an opportunity to test the systems. How sound our readiness is and how quick we are to adapt,” he said.
So far, he thinks Norway has done pretty well.
“I think we've been good at adapting. We have managed to follow the plans we have had so far and we haven’t had any big surprises,” he says.
“I think we have tried to take the right action at the right time. But this is also about fatigue in the population. We will have to do this for a long time and people must stay the course with us,” he says.
If that's enough, only time will tell.
“We don’t know how much we can dampen the spread with the actions we have taken now. We have systems where we measure the effects of what we’ve done so far on an ongoing basis, and we hope that what we’re doing is enough so that we don’t exceed the capacity of the health care system,” he says.
Translated by: Nancy Bazilchuk
———
Read the Norwegian version of this article on forskning.no
































