Battling cancer with light
An intense beam of light releases poisons introduced into dormant cancer stem cells.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
“Three, two, one, zero!”
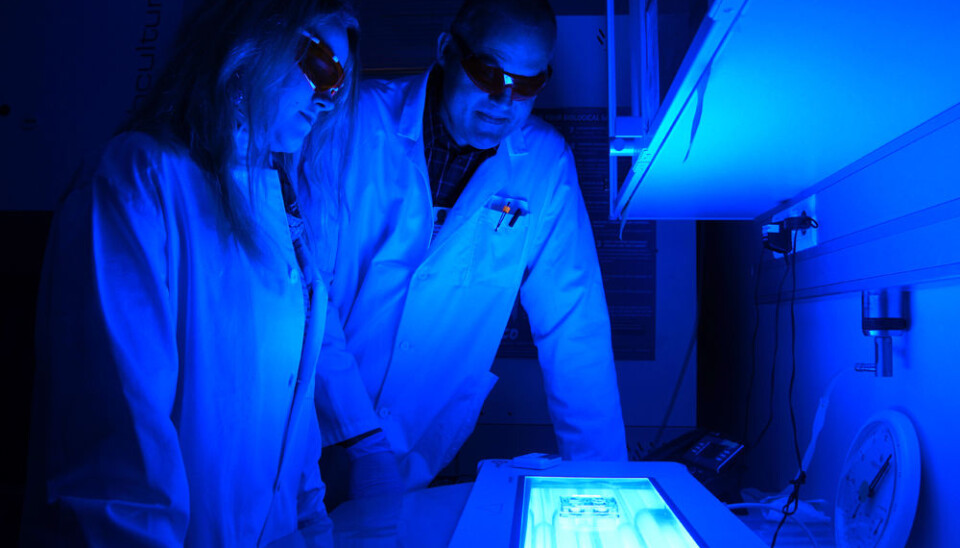
Pål Selbo counts down and Monica Bostad flicks a switch. The laboratory at the Norwegian Radium Hospital in Oslo is bathed in blue light.
Light fights cancer stem cells
Petri dishes containing cancer cells are illuminated on the glass table. The cells get their allotted seconds of light.
But the beams are a far cry from the ones used in radiotherapy at the Norwegian Radium Hospital.
Radium is made to emit radioactive beams that kill cancer cells. But Bostad and Selbo are using normal beams of light.
The blue light is not harmful in itself. But the method they have developed enables the light to release strong chemicals. These poisons can kill certain types of resistant cancer cells, called tumour or cancer stem cells.
The special type of drug delivery is called photochemical internalisation, or PCI.
It was developed in 1995 by Professor Kristian Berg. He now leads the team of researchers that includes Selbo and Bostad.

The story of PCI is a tale of cooperation between researchers and industry. Pål Selbo is a cell biologist and senior scientist working with the Radium Hospital and the firm PCI Biotech. Monica Bostad is a pharmacist and a PhD candidate.
But part of the history behind this kind of therapy goes much further back, to Mediaeval times, and the use of the traditional herbal plant garlic mustard. The leaves and roots of this flowering perennial, a member of the carnation family, were boiled and the extract was used medicinally to treat a host of maladies ranging from bronchitis to constipation and syphilis.
The substance used by Bostad and Selbo, a protein called saporin, is extracted from garlic mustard seeds. But don't let its humble origins fool you: Saporin is one of the strongest poisons known.
Related to ricin
Saporin is related to ricin, another toxic protein which unfortunately makes headlines and is sometimes used for nefarious political purposes. KGB agents were known to have used it to bump off defectors. Solitary terrorists have also used it now and then.
It’s one of the substances President Obama’s White House and the US Congress have to check for in incoming mail, for good reason. In June this year a Texan woman was indicted for sending them ricin-tainted letters. It has even made its way into popular culture, and played a role in the last episode of the television series "Breaking Bad."
Ricin strikes inside cells. The poison attacks ribosomes, which are the cell's protein factories. The cell's metabolism stop and the cell dies.
Saporin works in the same way, but needs help to get inside a cancer stem cell. Bostad and Selbo have a method for doing just that.
Behind enemy lines
The trick was getting saporin inside the cell membrane. The cell membrane is like a gatekeeper, letting selected substances in and out of a cell. Without this protection, a cell would be unable to absorb nutrients or release waste.
How do you trick the gatekeeper into admitting a chemical like saporin? You hook it up to an antibody.
The antibody with its load of saporin connects to a receptor on the membrane, a protein called CD133.
Some harmful cancer cells that are targets for destruction contain a lot this protein.
CD133 acts as a hatch behind the gatekeeper, a way through the membrane. It enables the saporin to be snuck inside the cell, like a secret agent behind enemy lines.
Trapped in the endosome
But the agent is soon captured. It becomes encapsulated in an endosome. The endosome is a compartment in the pathway from the cell membrane to the lysosome, a part of the cell responsible for its trash disposal.
In other words: The agent saporin is in deep trouble. It has to escape from the endosome.
The firm PCI Biotech has worked with the researchers to develop a weapon for saporin and other pharmaceutical products that get captured by endosomes.
Blows up the lysosome
Their weapon is called Amphinex. It is photosensitising agent, which means that it reacts to light.
Amphinex accompanies saporin into the cell. It attaches to the walls of endosomes and lysosomes, like explosive mines stuck to the hull of enemy submarines cruising in the cell fluid.
The photosensitising substance Amphinex explodes when it is hit by Bostad and Selbo’s beams of blue light.
Doomed cancer stem cell
The explosive in this case is oxygen. When struck by light, Amphinex transforms O2 into reactive oxygen species, compounds as well as singlet oxygen.
We tend to think of oxygen as a life-giving element. But oxygen is a double-edged chemical sword. Reactive oxygen species are chemically reactive molecules containing oxygen that easily combine chemically with other substances, sometimes destroying them.
This is what occurs inside the cells. The walls of the endosome and lysosome are simply ripped apart.
The agent saporin is then free and can go to work on the ribosomes. Protein synthesis stops. The cancer stem cell is thus doomed.
From glass to living organisms
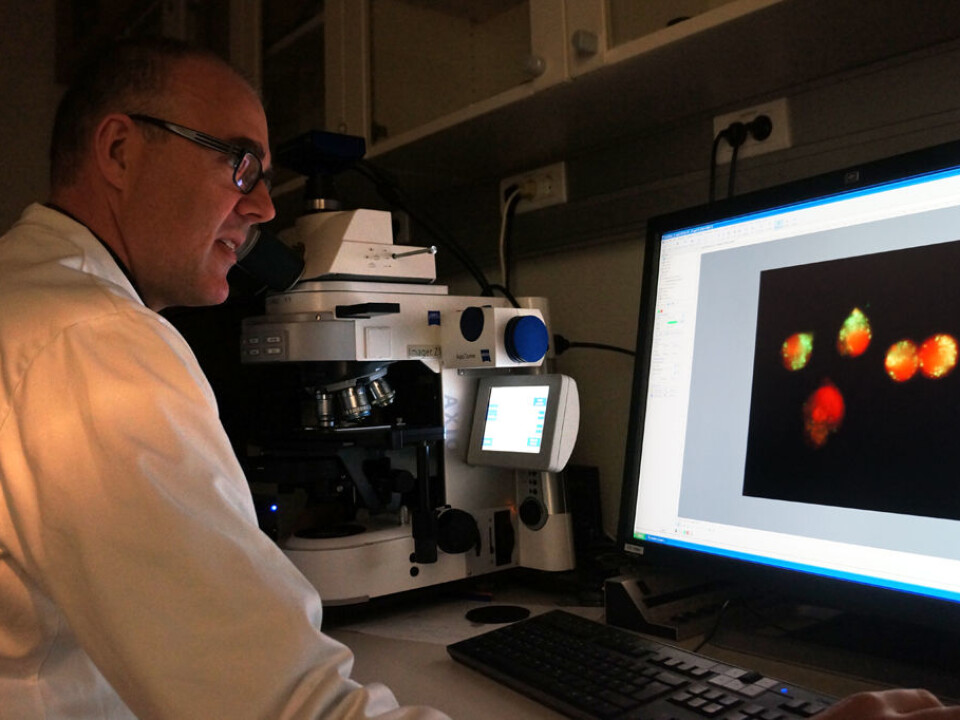
The method used by Selbo and colleagues to destroy the targeted tumour stem cells has only been proven in cell cultures in Petri dishes. This is what scientists call in vitro, in glass.
The next step is to show that the method can be used on laboratory mice – in vivo, in life.
Crossing fingers
As usual, the road here to clinical use for cancer patients is long.
Cancer stem cells containing CD133 are found in cancers of the colon, liver, ovaries, pancreas and brain.
Cancer stem cells are highly resistant. Like other stem cells, they have bulwarks against external attacks.
Cancer stem cells can survive efforts to destroy them with radiotherapy and chemotherapy. Just a few of these stem cells suffice to generate lots of new cancer cells, and thus spread – metastasise – throughout the body. The researchers stress that this is why it’s important to fight these particular cells, not just the bulk of cancer cells in a tumour.
The PCI method is effective against cancer stem cells, so it is promising. If Bostad, Selbo and their colleagues succeed, the survivability from several types of cancer could be much higher.
Translated by: Glenn Ostling