
Which smokers and ex-smokers are at greatest risk for lung cancer?
Researchers at NTNU are developing a new method for more accurately calculating the individual risk of lung cancer in smokers. A number of risk genes are baked into the model.
Lung cancer takes the most lives of all cancers. Each year, approximately 2.1 million people are diagnosed with lung cancer worldwide.
CT screening of selected people can increase survival, according to several studies. Many European countries are planning to introduce lung cancer screening.
The problem lies in selecting individuals who have the highest risk.
Only minority of smokers get lung cancer
Most people who get lung cancer are either currently smokers or ex-smokers.
But only a minority of smokers ever develop lung cancer. This means that the risk is unevenly distributed.
Why can some people smoke like a chimney for decades without being affected, while others who quit get lung cancer many years later?
Scientists have not known the answer.
But now researchers in Trøndelag county are learning more.
Over 20 genes increase the risk
Oluf Dimitri Røe, a professor at NTNU and senior physician in oncology at Levanger Hospital, is one of the researchers investigating various risk factors.
He has based his study on a large amount of data from The Nord-Trøndelag Health Study, known as the HUNT surveys, one of the largest health studies ever performed.
The HUNT study and a collection of ten studies from all over Norway showed that about nine out of ten people who develop lung cancer are current or past smokers.
“The goal was to find a method for selecting smokers with the highest risk, and avoid screening people who don’t need it,” Røe says.
Calculator computes risk
The study provided the basis to develop the HUNT Lung Cancer Risk Calculator, which computes individual lung cancer risk for smokers and ex-smokers.
Try the HUNT-calculator to calculate your personal risk of getting lung cancer here.
Røe recently presented an improved model of the calculator at the World Conference on Lung Cancer in Vienna, the newspaper Dagens Medisin recently reported (link in Norwegian).
In the new calculator, the researchers combined clinical data with the genetic fingerprints of 22 genes responsible for higher lung cancer risk.
Disadvantages of screening all smokers
The earlier that lung cancer is detected, the better a person’s chance of survival.
So why can't everyone who smokes or has smoked be offered screening?
“The problem is that lung cancer screening is currently done with a CT scan of the lungs. Finding very small changes that might be benign could yield a so-called false positive result, which could lead to unnecessary interventions,” says Røe.
Some people might have cancer that isn’t aggressive and doesn’t need surgery, he explains.
Having repeated CT examinations also entails a small risk of cancer. The capacity of radiologists and CT scanners, and the balance of cost-benefits are also factors that need to be considered.
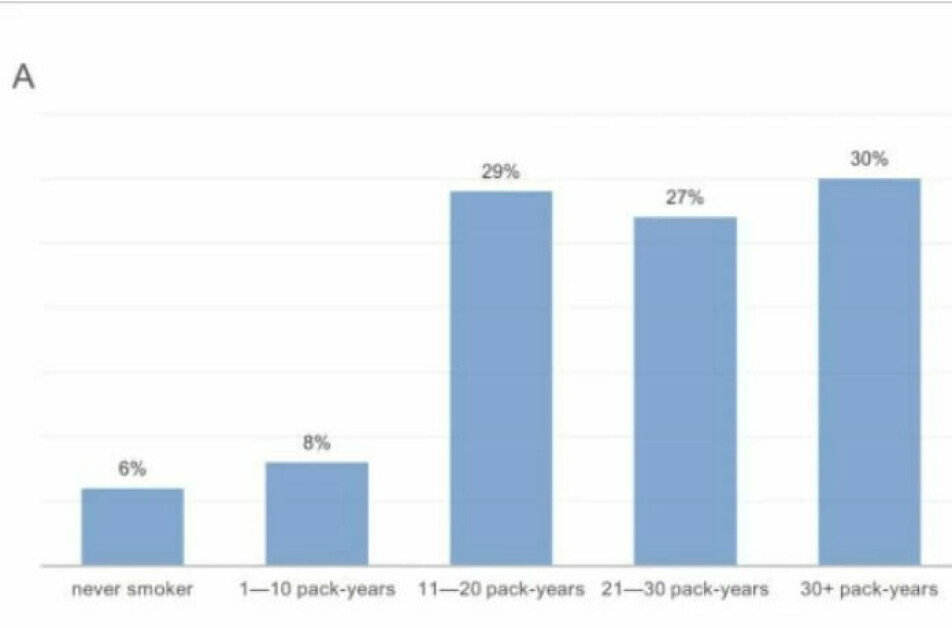
Only 3 out of ten of patients with lung cancer were heavy smokers for 30 years
“That’s why it’s so important to select the right people, and this model can do that,” Røe says.
Internationally, a big discussion revolves around which criteria should be used for screening candidates.
The model uses simple criteria for selection. They include: age 55 to 75, greater than 30 pack-years (which means 20 cigarettes a day per year), and less than 15 years since quitting smoking.
“We found that only 30 per cent of people who received the diagnosis had smoked 20 cigarettes a day for more than 30 years,” says Røe.
Screening recommended for every fifth smoker
The old criteria excluded more than three quarters of the individuals who would develop lung cancer.
“A lot of studies, including ours, show that a calculator with several variables is the right way to go,” says Røe.
With their first calculator, the HUNT Lung Cancer Risk Calculator, the researchers were able to predict 81 per cent of lung cancer cases by screening only 22 per cent of smokers.
Just over one in five smokers and ex-smokers need to be screened, according to the model.
New calculator detects three times as many cases
Using the usual criteria, researchers detected only 24 per cent of the cases.
“We’re finding 3.3 times as many cases with the new calculator,” says Røe.
Similar calculators have been developed in the past, but they have only included heavy smokers.
No one has previously included younger people, individuals who smoke less or those who have stopped smoking in the calculation.
Coughing increases risk
How much and how long a person has smoked is not the only determining factor for their personal risk of lung cancer.
Periods of daily coughing during the year are also an important factor.
“If you smoke indoors or are exposed to passive smoking for hours a day, the risk also increases – in contrast to smoking outdoors,” says Røe.
Thin people are also at extra risk.
“People who smoke and have a low BMI (body mass index) also have an increased risk, although we don’t know why,” says Røe.
This factor contrasts with a number of other types of cancer, where a high BMI increases the risk.
Worse to smoke a few cigarettes for a long time than in a short time
“We also found that having smoked a lot for short periods is less of a risk than smoking fewer cigarettes daily over several years,” says Røe.
The risk also increases with age because it takes many years to develop cancer after you start smoking.
For people who have put out their cigarettes, the risk decreases quite quickly and with the number of years since quitting. But they will still carry a certain risk of lung cancer.
The HUNT Lung Cancer Model, which calculates lung cancer risk, was published in the journal EBiomedicine in 2018.
One per cent risk is high
If the calculator computes that you have a one per cent risk of getting lung cancer, that might seem low to a lot of people.
But that estimate only indicates the risk of cancer for the next six years.
“It’s actually a high risk,” says Røe.
He compares the calculation to flying.
“Would you board a plane if you knew that one in a hundred planes crashed?”
He stresses that the calculator is not a substitute for a doctor's visit. The most important step a smoker can take is to quit smoking for good.
“A calculator that computes your personal risk over the next six years can also inspire smokers to quit,” Røe says.
22 genes increase risk
The researchers have now improved the effectiveness of the risk model even more. In addition to smoking habits, genes also play a role in the risk of lung cancer.
“In the HUNT study, we analysed the gene profile of all the participants, since genetics are also linked to lung cancer,” says Røe.
Røe and his colleagues have taken the variables from the calculator and combined them with the 22 risk genes.
The work is part of Olav Toai Duc Nguyen's doctorate. He is also a senior physician in oncology at Levanger Hospital and a colleague of Røe.
The researchers are collaborating with the University of Tromsø and the University of Crete.
Every sixth smoker or ex-smoker is at high risk
The researchers have managed to further narrow down who should be offered a CT scan of the lungs.
“We detected 30 per cent more people at high risk with this model,” says Røe.
The model detects the 16 per cent of smokers and ex-smokers with the highest risk. By selecting them, 73 per cent of lung cancer cases in the next six years can be detected, according to Røe.
The research team believes this model is much more effective in selecting people for lung cancer screening than the criteria being used in Europe and the USA today.
The researchers have tested the model against a larger population-based cohort from Tromsø. Now all that remains to be done is to validate against a larger international cohort.
Request a genetic test?
To use the new model on individuals, a person has to have certain risk genes mapped.
“In theory a person could use the simplified calculator and go to the doctor and ask for a genetic test, but first we need to develop a separate kit for the analysis and a calculator app that explains what the results imply,’ says Røe.
He estimates that this could likely become an offer in the healthcare system in two to three years.
“The goal is for people to have the option to screen their lungs if the risk score shows that it’s necessary,” he says.
The researchers do not know how widespread these genes are in the population.
The new model has been named the HUNT-Lung-SNP model. Røe and his colleague presented it at the World Conference on Lung Cancer in August this year.
Reference:
Maria Markaki et.al.: A Validated Clinical Risk Prediction Model for Lung Cancer in Smokers of All Ages and Exposure Types: A HUNT Study. eBioMedicine, 2018.
———
Read the Norwegian version of this article at forskning.no
































