What mammogram images tell us about breast cancer risk
Breasts with dense fibroglandular tissue and less fatty tissue increase a woman’s risk of breast cancer. At the same time, this knowledge hasn’t translated into greater follow-up for these women.
It is well known that women with dense fibroglandular tissue in their breasts have an increased risk of breast cancer, compared to the average. But there’s no way for a woman to know if her breast tissue puts her at increased risk without an image from a mammogram.
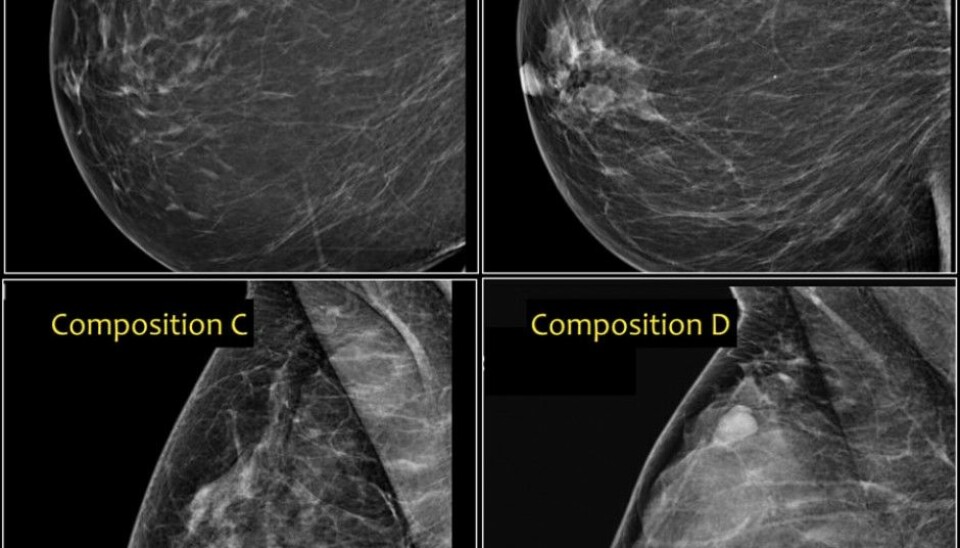
Dense fibroglandular tissue in the breast is made up of milk glands and connective tissue. It will appear as areas of white or light grey in mammography images. Fatty tissue, by comparison, appears black or dark grey in the images. Essentially, lighter images mean denser tissue, which doctors and radiologists describe as mammographic density.
Since the risk of breast cancer is greater in women with a high proportion of fibroglandular tissue (and thus greater mammographic density), Norwegian researchers have wondered if they can use mammographic density as a way to increase their accuracy when checking for tumours in the country’s mammography screening programme, which is offered to women older than 50.
Should women with breasts with greater mammographic density be offered more frequent screening or other screening methods in addition to mammography? This is called stratified screening, and is offered in the United States, for example.
Nataliia Moshina, a medical doctor and PhD candidate, wanted to see whether the Norwegian mammography programme should be modified in view of this information.
The current understanding of mammographic density and cancer risk is mainly based on information from women with breast cancer. Researchers need more information about healthy women whose breasts also have high mammographic density.
Bigger tumours
Moshina’s research was based on data from women who participated in the Norwegian Mammography Programme for 20 years, between 1996 and 2015.
The tumours detected in the women with "dense" breasts had a larger average tumour diameter. A larger proportion of these tumours also had spread to lymph nodes in the armpit, compared to women with fatty breasts.
Both of these characteristics are of major importance in a woman’s prognosis. Women whose tumours are large and have spread have a lower likelihood of being cured of the cancer and surviving.
"There is a lot to suggest that screening for breast cancer may be better in the long term if you take into account mammographic density," Moshina says.
Standardization still needed
Nevertheless, Moshina says that it doesn’t yet make sense to offer women with mammographically dense breast tissue more follow-up.
“Unfortunately, we still don’t know enough. For example, we still have no good, objective way to measure density,” she says. “We need a standardized tool before we can safely and effectively assign women to different risk groups based on breast density.”
The current method relies on the judgement of the radiologist who reads the mammogram and makes a visual estimate of how much of the breast is composed of dense, fibroglandular tissue.
“This is a subjective assessment method that creates variations in how images are judged, based on the individual who does the assessment,” Moshina said.
Another factor that contributes to variation in breast density assessments is that radiologists are supposed to be focused on looking for signs of breast cancer in the image, not assessing density per se. They also have to work quickly.
Software may offer a solution
Moshina also explored the use of software to read the density of mammography images. A computerized system should in theory offer a standardized measurement method.
“The results showed that the automated method was comparable to the subjective methods used by radiologists. However, the automated method was not without challenges, "said Moshina.
Her doctoral thesis concluded that we need to know more about measurement methods for mammographic density before this risk factor can be used to change Norway’s screening programme.
References:
N. Moshina: Understanding the role of mammographic density in a population based breast canser screening program: A step towards stratified screening for breast canser in Norway? Doctoral thesis, Universitetet i Oslo, det medisinske fakultet, 2017.
N. Moshina mf: Breast compression parameters and mammographic density in the Norwegian Breast Cancer Screening Programme. Abstract. Pub. Med. 2. november 2017. 2017 Nov 2. doi: 10.1007/s00330-017-5104-5.
-------------------------------------































