More colorectal cancer in Norway than elsewhere in Europe
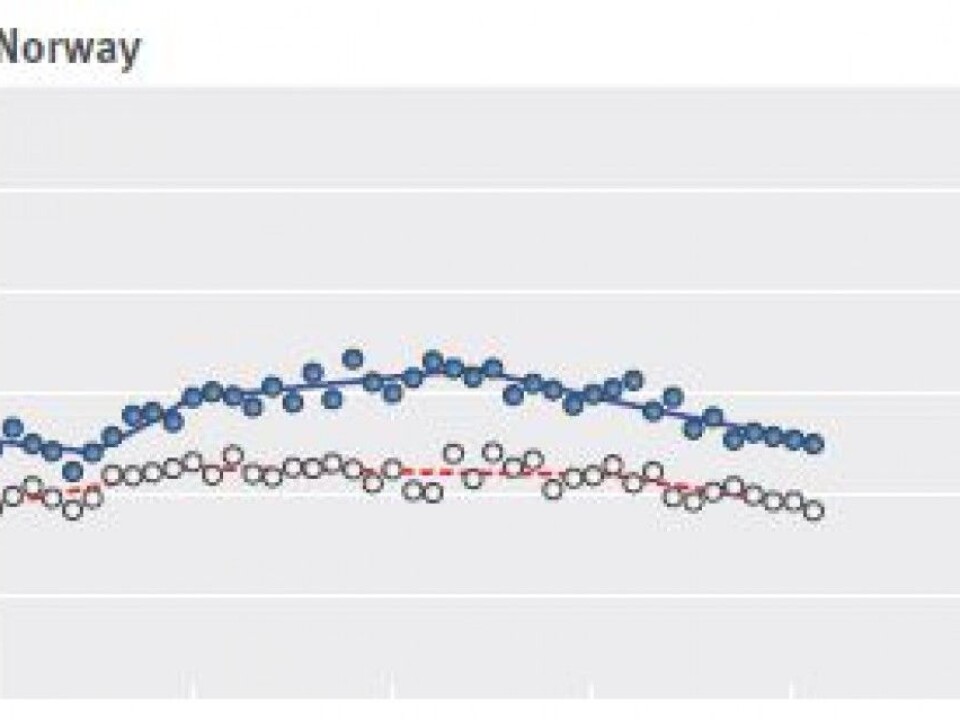
While fewer Norwegians are dying from colorectal cancer now than twenty years ago, other countries have done a better job in cutting mortality from the disease.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Colorectal cancer deaths have dropped in a number of European countries, particularly in northern and western Europe. But there is considerable disparity in mortality levels between different European countries and between men and women, a recently published study on the deadly disease reports.
Colorectal cancer is the second most commonly diagnosed cancer in the world. In Europe, only lung cancer kills more people each year.
In Norway, 3500 people are diagnosed with either colon cancer or rectal cancer each year. Four out of ten will die from the disease within five years. But mortality varies greatly and depends on how far the disease has spread before diagnosis. Prospects for rectal cancer are somewhat brighter.
New treatment methods have also led to more cures and longer survival times compared to 20 years ago.
Women see the most improvement
Researchers reported in The BMJ (formerly the British Medical Journal) that mortality in the 34 European countries evaluated in the study increased by six per cent among men, but fell by 15 per cent in women between 1989 and 2011.
The researchers used figures from the World Health Organization's mortality database from 1970 to 2011. They paid special attention to what happened after 1988, when there were major changes in screening and treatment effectiveness.
The study reported the greatest decreases in mortality in the 27 EU member states, where mortality fell by 13 per cent in men and 27 per cent in women during the study period.
Even though fewer people in Norway are dying of colorectal cancer now than in the past, a number of countries have had far stronger declines in mortality than in Norway.
High prevalence in Norway
Norway has a very high incidence of colon and rectal cancer.
“In Norway, we have had an unfavourable development - colorectal cancer has increased more than in many other countries. While fewer are affected by this cancer in Norway than a few decades ago, we are now at the top in Europe,” says Bjørn Møller, a researcher and head of the registry division at the Norwegian Cancer Registry.
But Møller and other researchers do not know why this is the case.
“It’s a good question. It probably has to do with lifestyle factors,” Moller says.
High incidence, but good treatment
Norway’s mortality numbers can be explained in part by the combination of an increased incidence of the disease over the period, combined with relatively good treatment since the 1970s, said Morten Tandberg Eriksen, head of the Norwegian Gastrointestinal Cancer Group.

“Other factors, such as lifestyle and screening programmes can also play a role,” said Eriksen, who is also head of the Gastric and Children’s Surgery Division at Oslo University Hospital.
Limited Norwegian screening programme
The countries with the greatest decline in fatal colorectal cancer also seem to have the greatest degree of screening, according to the BMJ study.
Norway does not have the kind of nationwide screening programme for colorectal cancer that is found in many other countries. But the country has a ongoing pilot project on screening that started in 2012.
A screening programme is being offered to a sample of 140 000 inhabitants between the ages of 50 and 74 from Østfold, Akershus and Buskerud counties. The pilot started in 2012 and ends in 2018.
“Participants will either be asked to submit stool samples where researchers look for invisible blood, or to be examined in the lower part of the colon with a endoscope. Those who have signs of early stage cancer or cancer, receive a follow-up colonoscopy, which is an examination of the entire colon using an endoscope,” says Thomas de Lange, who is head of the pilot project at the Cancer Registry.
He says it too early to say which type of screening works best.
“It will take another 10-15 years before we see how this affects the incidence and mortality for colorectal cancer,” he said.
Deep reductions in some countries
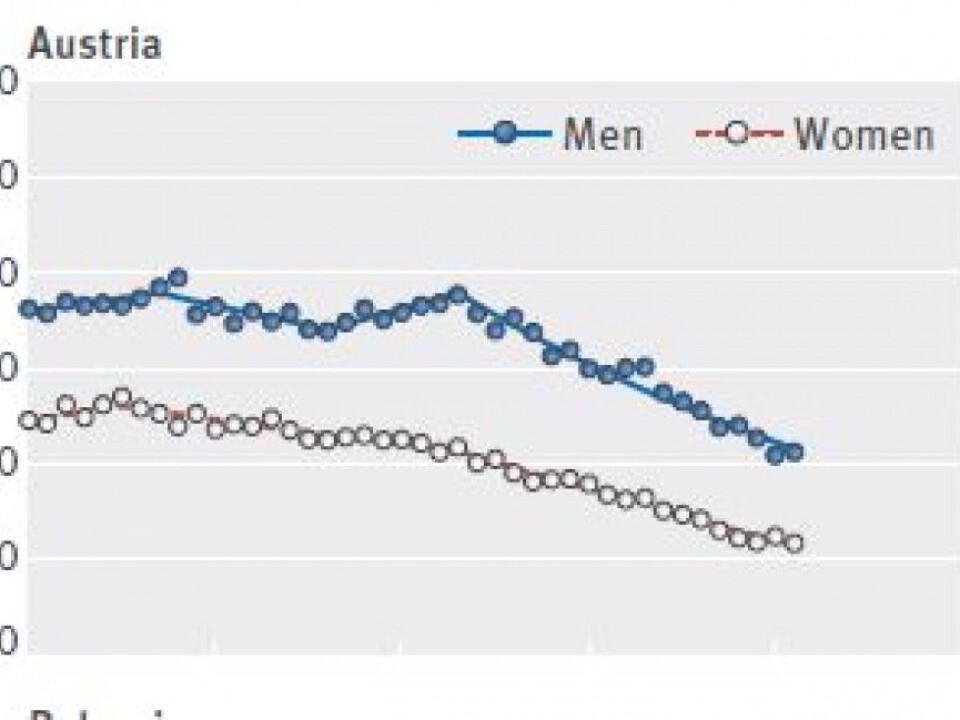
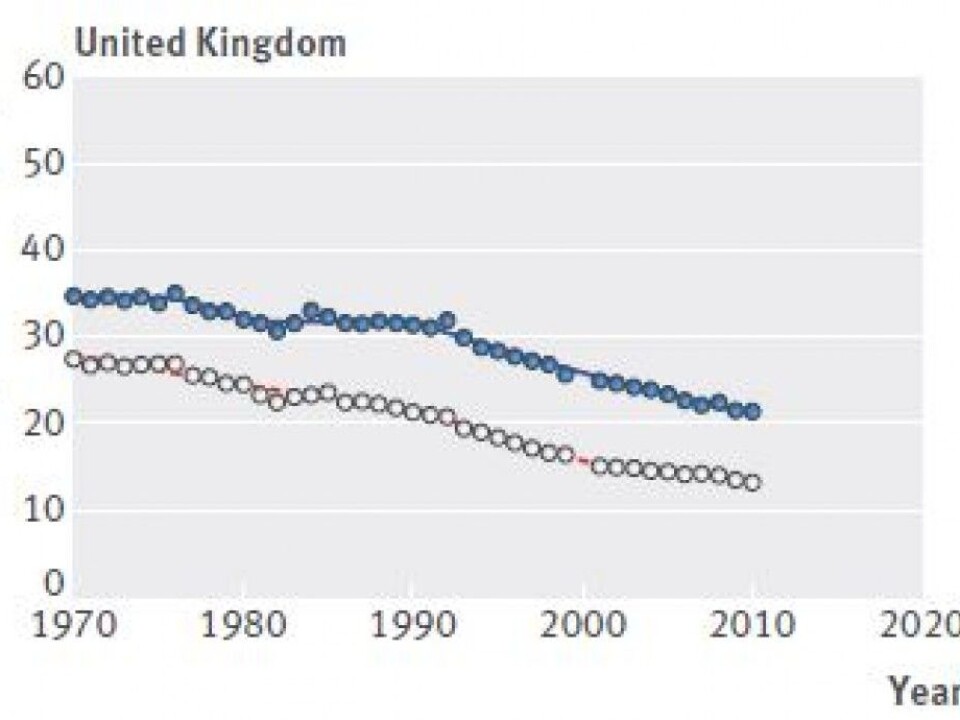
Austria, Switzerland, Germany, Britain, Belgium, the Czech Republic, Luxembourg and Ireland all saw deep reductions in mortality from colorectal cancer, the researchers report.
”The UK is one of the countries that has a systematic screening programme,” says de Lange at the Cancer Registry.
In these countries, mortality from colorectal cancer has fallen by more than 25 per cent among men and 30 per cent among women. In the Netherlands and Sweden, in contrast, mortality rates decreased by less than 17 per cent for both men and women.
The BMJ study says this is consistent with the idea that countries with the largest reductions in mortality also seem to have the highest level of screening. Access to colonoscopies in the Netherlands is more limited than in France, Austria and Germany, the researchers noted.
Screening well established in some countries
Screening for colorectal cancer involves widespread testing to find colorectal cancer or precancerous lesions.
The BMJ article reports that research showing that regular testing of stool samples could reduce the risk of death from colorectal cancer encouraged several European countries (such as France and the UK) to undertake this kind of screening.
Similar research “supporting the effectiveness of colonoscopy screening helped establish endoscopy as the primary screening procedure for colorectal cancer in the USA as well as in many European countries (for example, Austria, the Czech Republic, Germany, and Poland),” the researchers wrote.
In 2013, Norwegian researchers also stated their support for the idea that screening for colorectal cancer saves lives. But other Norwegian researchers have found that some patients who have had polyps removed from their colons undergo unnecessary follow-up checks for colorectal cancer.
-------------------------------------
Read the Norwegian version of this article at forskning.no
Scientific links
External links
Related content