Protein found that can save colon cancer patients
Patients under treatment for colon cancer who have only a small amount of a certain protein in their tumour are at a high risk of relapse. New information about these tumours can be used in targeted treatment that saves lives.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
A mounting number of Norwegians are being diagnosed with colon cancer– the fourth most common cancer type in the country.
Most patients can expect a good prognosis if this cancer is diagnosed in an early stage. Eight out of ten can be healed through surgery alone if the cancer is detected before it metastasises to lymph nodes.
But up to 25 percent experience a relapse and to date doctors have lacked sufficient ways of determining which patients are in the danger zone.
Division into stages
Cancer patients have long been divided into various clinical stages according to how far the disease has progressed.

In stage 1 and 2 the tumour is local.
In stage 3 it has spread to lymph nodes.
In stage 4 it has spread to other parts of the body.
The discovery of biomarkers has enabled physicians to subdivide patients into further groups within each stage and thus provide treatments which are more individually based.
Found less protein in the tumours
Researchers at Oslo University Hospital, the Radium Hospital, have found a new method for identifying patients who run high risks in stage 2.
The researchers found that the tumours of patients who later suffered relapses totally lacked or had little of a specific protein that is vital for healthy cells.

This discovery makes it easier to spot the patients who are most in jeopardy. These can thus offered subsequent treatment, such as chemotherapy or targeted medications, after the surgical removal of tumours.
New characteristics of menacing tumours
Molecular Biologist Jarle Bruun of the University of Oslo recently got his PhD in characteristics of colon cancers.
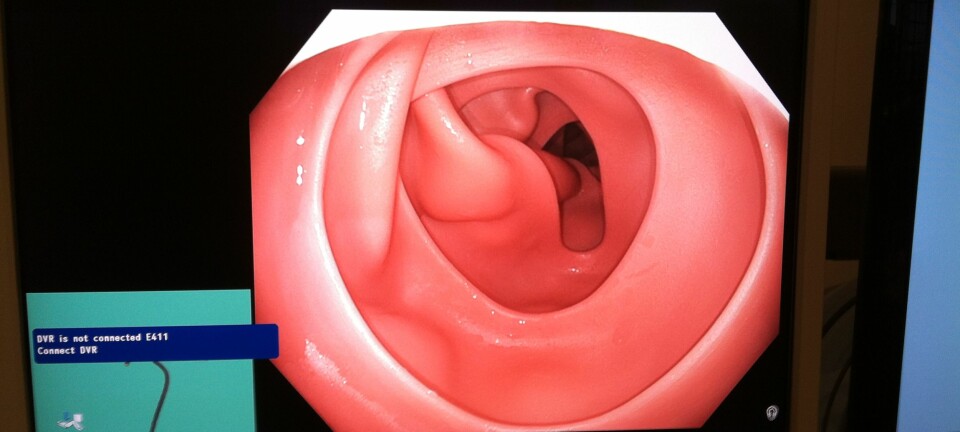
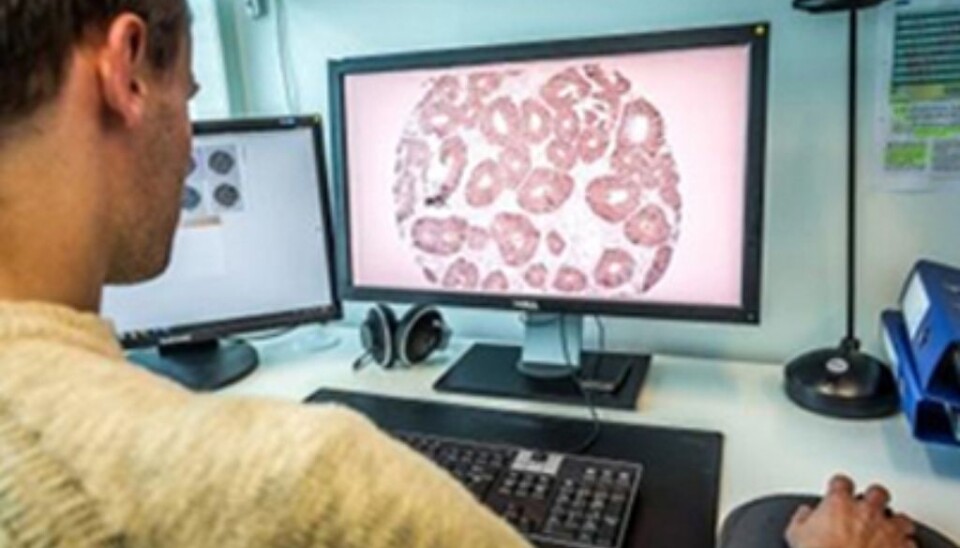
Bruun made ultrathin slices of tumours removed from colon cancer patients. The tumour tissue was preserved in formalin, secured in wax and then sliced.
When magnified images of these slices were analysed with the help of a computer, amounts of a particular, brown protein could be made conspicuous.
The medical researchers found noticeably smaller amounts of the protein in tissue samples from patients who suffered relapses, as compared to patients who regained their health.
“The absence or reduction of a certain protein is associated with a poor prognosis,” says Professor Ragnhild A. Lothe, who was Bruun’s advisor in his doctoral work. The protein is called RCC2 and regulates a gene by the same name.
Bruun looked at data stretching back to 1993 and compared patients whose cancer was nipped in the bud with ones who suffered relapses.
Better follow-ups
“This is a link in a systematic effort to establish a set of biomarkers that give us an early warning about prognoses. This enables us to sort patients into sub-groups according to risks,” explains Professor Ragnhild A. Lothe.
Lothe leads the Department for Cancer Prevention at Oslo University Hospital, the Radium Hospital.
The division into such groups makes it easier for doctors to channel resources and special treatment to the patients with higher risks.
No tumours are identical
Bruun has also conducted experiments indicating that the protein is key in the development of colon cancer.
“All cancer tumours are individual. We can find mutations in some tumours, in other words, deviations in their DNA material. In others we find that the tumours lack a specific protein,” explains Lothe.
Treatment according to risk
Future cancer treatment will be more oriented toward fighting the disease in earlier stages.
It’s essential for doctors to determine which patients need preventive treatment. Those who run a high risk of relapse will be given treatment that is more precisely targeted and can draw advantage from experimental treatment methods, according to Lothe.
“But we mustn’t forget that even if we identify all who are at high risk, there is no telling how many of them will benefit from additional treatment,” emphasises Lothe.
Not a routine
Up to now, treatment has been administered on the basis of which cancer state a person has when the disease is diagnosed. Cancer patients with a spread to the lymph nodes, usually receive chemotherapy after their surgery.
But patients in stage 2 do not routinely get such additional treatment after their operations, even though as many as quarter of them suffer relapses.
“This is because so far we have not known which of them are at risk. If we treat everyone in this category, very many will be subjected to treatment for the sake of the few, according to earlier studies,” says Lothe.
Treatment needs to be adapted to give the maximum effect for individual patients. This can be a combination of targeted medications based on the characteristics of the tumour, and/or chemotherapy.
Developing tests
Work has now been started on developing a test for clinical use. But first the test needs to be confirmed by other researchers.
Collaboration has started with a cancer treatment centre in the USA.
“We hope the test will be tried and confirmed so that it can be put to use,” says Lothe.
Few biological markers are currently utilised for guidance in choice of treatments for colorectal cancer. The ones used are for patients with a metastasis to other organs.
------------
Read the Norwegian version of this article at forskning.no
Translated by: Glenn Ostling