
Insufficient follow-ups of cancer survivors
“It’s like sending people off to war and declining to take care of them when they come home,” says Norwegian physician and psychiatrist.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
A close acquaintance thought it odd that I could sleep for hours and hours and never be rested. So she started to search the web to look for reasons. She found an article about fatigue which I brought along to my family doctor. He agreed with what was written there and it was almost as if it were written about me.
Anita Aga Abu Mohor wrote the above to the Norwegian ScienceNordic.com’s Norwegian partner forskning.no. She was diagnosed with cancer at age four and treated for the disease until she was six. She is now 26 and is aware of how her life has been marked by the treatment she received as a young girl.
She has battled with concentration problems and psychological and physical ailments. The fatigue she suffers is a typical late effect of her cancer treatment.
Cancer treatment often involves chemotherapy, radiotherapy and various other forms of treatment lasting for years. When a child gets cancer the health services do all that is possible to cure it, and fortunately the battle is often won.
But cancer treatment is harsh on the body and many patients suffer long-term side effects – known as late effects.
In 2011 about 30,000 persons in Norway were diagnosed with cancer. A mounting number of these victims – children and adults – survive the disease, thanks to new medical advances which are constantly being made.
However, with steadily more long-term survivors, the ranks of ex-cancer patients suffering serious later effects are also increasing.
Consequently more people need to be offered schemes to follow them up for years afterwards. But doctors and cancer survivors say such schemes are insufficient, or even lacking altogether.
Chronic ailments in adulthood

People who experienced cancer as a child think they would benefit from some sort of follow-up at least once every five years, according to a Norwegian study which is still unpublished. As part of the study researchers created focus groups among a selection of 34 persons who had cancer during childhood.
In the current system, childhood cancer patients are the responsibility of paediatric health services until the age of 18. After that, all their health issues have to be channelled through their designated general practitioner (GP), just like any other persons living in Norway.
If no late effects are diagnosed before age 18 the Norwegian health services lack a systematic long-term scheme for the prevention and treatment of such side effects among these patients.
The problem is that late effects often tend to crop up long after cancer treatment ended.
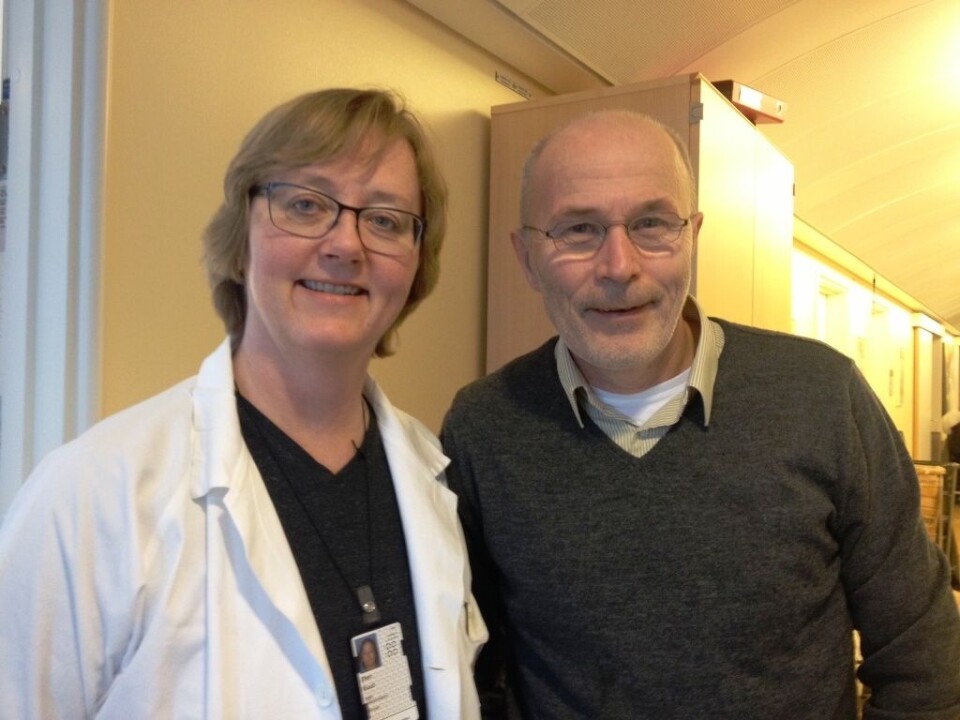
Jon Håvard Loge is highly critical about the way survivors of childhood cancer are currently cared for.
Loge is a doctor and specialist in child and adolescent psychiatry. He also leads the National Resource Centre for Late Effects after Cancer Treatment at Oslo University Hospital.
“We see we’re lacking something here in Norway. Both Sweden and Denmark have resource centres where anyone who survives cancer, whether as an adult or as a child, has access to a special service,” says Loge.
“I don’t think we can circumvent this in Norway. Some people have very complicated conditions requiring visits to special clinics.”
He draws the support of Ellen Ruud, who is chief physician at the Department of Paediatric Medicine of the Oslo University Hospital.
“What we are talking about to avoid late effects is no more expensive than the costs of treating them once they occur,” says Loge.
Insufficient knowledge of own risks
A study by researchers at Oslo University Hospital, Radium Hospital, showed that 66 percent of the survivors of childhood cancer knew nothing at all about the risks of late effects after their cancer treatment.
Anita Mohor was not initially clear that her health problems later in life were linked to the treatment she received as a child. She writes:
It took a long time before I realised that the cancer was the cause, because we were not told this could happen.
Nor are health personnel, GPs and the Norwegian Labour and Welfare Service (NAV) employees sufficiently aware of problems such as cancer-related fatigue, according to a study made in connection with PhD work at the University of Tromsø.
So the family GP might not be the best person around for catching the initial late effects in patients and informing them how they can prevent some of these, for instance with healthy lifestyles.
Together with a research group in Trondheim, Jon Håvard Loge and Hanne Catrine Lie of the Department of Behavioural Sciences in Medicine at the University of Oslo are working on a research project involving interviews with GPs and oncologists.
They hope to find out whether it is practical to start a system for long-term follow-ups of those who need them.
Off to war
As many as two out of three survivors of cancer in childhood have at least one chronic health problem as adults.
But the problem of late effects essentially looms over anyone who has survived a long time after their cancer was cured.
“What we do today is akin to sending people off to war without taking care of them when they return home. The ones involved have serious health problems,” says Jon Håvard Loge.
GPs will be able to tackle the follow-ups needed by most of the people who were treated for cancer as children.
But some 10-15 percent of the 220 children who are diagnosed with cancer each year in Norway will suffer severe late effects and need treatment from specialists. Others will fall between the two categories and will need a combination of special check-ups by GPs and specialists.
Lack of check-ups and information
Anita Mohor’s story shows how the absence of systematic follow-ups can be experienced after a person reaches the age when paediatric care no longer has responsibility for their care.
I was called for a check-up at Haukeland University Hospital each year and blood samples were taken until I was 15. At these check-ups we talked about how things were going right then, but nothing about the future. I was not followed up after that. Now over 20 years have passed since I got sick and hopefully things have changed. I suppose they didn’t have the information they needed back then. I hope that children are followed up better now than I was.
Mohor was routinely examined until the age of 15 but does not think she was given enough information about the late effects she could experience later on.
Researchers ask whether we can improve routines for informing survivors of cancer in childhood to help them prevent late effects.
Lacking contacts
The Norwegian researchers think that resource centres, or survivorship clinics, could help cover the need for such follow-ups.
Lie explains:
“A woman said it was like a jungle. She didn’t know who she should contact about things she wondered about. Her GP didn’t know much about late effects and she didn’t feel could call the children’s ward at the hospital and say ‘Hey, remember me?’”
“Evidently these persons have no natural place to turn, which a specialist facility would be,” says Lie.
Anita Aga Abu Mohor hopes that follow-ups will improve for future ex-cancer patients:
I think that if follow-ups could be better my life would be totally different today – mentally and physically. I think it’s essential to research more about how it can mark the rest of cancer patient’s life. I would really like to see my story used to help others in the same situation to show that life won’t be a bed or roses even though you been so lucky to get a new lease on life. And you might not be like other people. While other children played and had fun, you were fighting a life-and-death struggle.
------------
Read the Norwegian version of this article at forskning.no
Translated by: Glenn Ostling






























