Fighting Cancer Cell Resistance to Radiotherapy
Researchers have discovered how cancer cells become resistant to radiotherapy. This means that they can also figure out how to turn it off.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Chris Smith from the Naked Scientists, a British science radio show, recently spent some days in Oslo interviewing Norwegian scientists.
Here he talks to Nina Edin and Erik Pettersen, who study Biophysics and Medical Physics at the Department of Physics, Oslo University
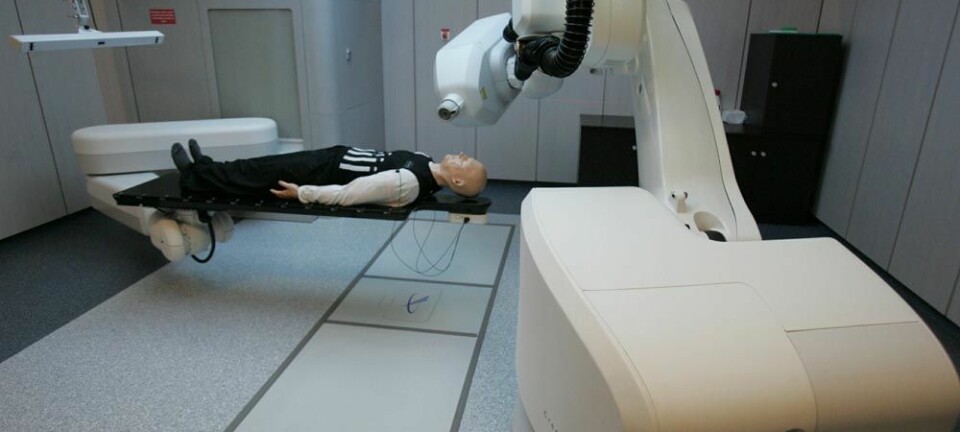
Chris: One very effective cancer treatment is radiotherapy, but this can have side effects when healthy tissue is also harmed, and that's because although most cells can be killed by very small amounts of radiation, the dose has to be high enough to prevent cancer cells becoming resistant to the treatment. Now though, Nina Edin and Erik Petterson have discovered how cancer cells become resistant and how to turn this off.
Nina: About 80 percent of all cell lines that have been investigated and, we believe, most normal tissue, has a property which makes them very responsive to radiation doses at about 0.3 gray which is about a 10th of the normal dose you give in radiation therapy.

So, if you can exploit this feature then you can give much smaller doses altogether and spare the patient from the radiation to the normal tissue.
Chris: Okay, do we understand the mechanism and are we in a position to put cells into that hypersensitive state, so that we can use very low doses of radiation to destroy them without having to do lots of other damage to healthy tissue in the body?
Nina: The problem is that when you give a small dose, then you induce a resistance to the next level dose.
Cancer cells detect radiation
Chris: So you give the small dose, you will wipe out some cells, but there will be a small hard-core group left behind that you won't get rid of, and moreover, they will be resistant. Then the next time you come in with another small dose, they're just not going to be destroyed. So how can we get around that?
Nina: Well, what we really have discovered is that something is secreted into the medium that can be affected by low dose irradiation, but not by high dose irradiation.
Chris: You're saying that cells have an ability to detect radiation at a low level, using a receptive molecule which then leads to the secretion of a factor which then, in turn, renders the cells resistant thereafter.
Nina: Yes, that is what I say and we have found the mechanism in the cells that keep this factor of secretion going and we’ve found a way to inhibiting this mechanism.
Chris: What are the chemical nuts and bolts that are doing this? What are the molecules that are doing it?
How to stop the resistance
Nina: The molecule that induces the resistance is TGF Beta 3 which is Transforming Growth Factor 3. The mechanism depends on INOS – Inducible Nitric Oxide Synthase and if we inhibit the effect of this molecule, we can stop the whole process and reverse the cells to the original hypersensitive state.
Chris: So what locks that effect in the cell?
Nina: It has to do with how the TGF Beta 3 works because it is only active when it is not bound to a molecule called Lap. So this Lap inhibits the effect of the molecule and it’s sort of a system to control the activation of it.
So what happens is that nitric oxide synthase produces nitric oxide and these nitric oxides take away the Lap so that this cannot re-associate with the TGF Beta 3, and then this remains active inside the cells and starts some other processes that make it – that all go around like a self-sustaining mechanism.
Chris: So putting that together, you have a small amount of radiation and that triggers the activity of INOS – Inducible Nitric Oxide Synthase – enzyme which makes some nitric oxide that removes the Lap molecule which activates the TGF beta molecule and that then triggers a locked-in change in the biochemistry of the cell, rendering it resistant to more radiation.
So if we block those actions then the cells would remain potentially hypersensitive to these very low doses of radiation. So Eric, how could you use this knowledge?
Useful knowledge
Erik: So far, we have been talking about cancer here, but this could have some influence also above or in other areas. TGF beta then seems to be able to turn off hypersensitivity. And for a person who has been, for example, experiencing irradiation, that could be very positive because that would often be small doses and if you could for example increase TGF beta 3 in some way after a very small dose, that might actually influence the response of this irradiation.
So, this could have some influence. We don't know this yet, but this could also have some influence in other areas than just cancer research.
Chris: If we had a way of addressing the signal to healthy tissue, we could protect healthy tissue. We could leave cancerous tissue vulnerable and this means that anti-cancer therapies like radiotherapy could be made much more effective at much lower doses.
Erik: Yes. By targeted administration for example, that could be a possibility. The important thing is that we have sorted out the mechanism which influences radiation responses at very low radiation doses.
A kind of stress response
Chris: And Nina, why do you think cells have this anyway? What’s it there to do, this mechanism normally? Why has evolution selected it?
Nina: That's a good question. I'm not sure. I think it does more things than we know yet, so I'm not sure that this only addresses hyper radiosensitive. I think it’s a kind of stress response, but one thing I didn’t say was that we have also tried to administer the TGF beta 3 after irradiation and it has an effect even four hours after they've been given the radiation. So it works backwardsm, which also is interesting if you have accidents.
Chris: And what could be the consequence of deactivating that signalling in healthy tissue if you block the ability to see TGF beta like that. Will the cells in any way suffer?
Erik: This is a very good question because you know, when cells respond by hyper radio sensitivity, it could be a normal response just to get rid of cells which have got some radiation damage, just to get rid of them. If the damage is not too bad, they can be easily restored by stem cells, from stem cells.
But if the damage is going on for a long time then they have the possibility to turn off the hyper radio sensitivity, do the repair and maintain the tissue by taking care of the cells. So, this could be a normal process which has some meaning in the restoration of tissues in general and we have some indications that this protection - we should call it protection of course - not only works against radiation but also against some toxic chemicals. So, it’s a more general stress factor than just radiation.
Chris: Erik Pettersen and Nina Edin.
------------------------