New medicine can stop autoimmune disease in mice
A new substance causes the immune system to stop attacking its own cells. An experiment with mice now shows that the drug prevented diseases similar to arthritis and type 1 diabetes.
Autoimmune diseases impact millions of people.
A report from 2015 estimated that between three and five per cent of the world's population has an autoimmune disease. There are over 80 different types of disorders, such as type 1 diabetes, celiac disease, Crohn's disease, multiple sclerosis, arthritis and psoriasis.
Although these disorders may manifest themselves very differently, they have one thing in common: they are due to the immune system attacking and destroying the body's own cells.
Today's treatment in many cases involves suppressing the immune system. But the effects of the drugs are often broad and suppress significant mechanisms in the immune system – including mechanisms we need to protect ourselves from threats like viruses, bacteria and cancer.
This means that the medications can have serious side effects, and it points out that we need new and better treatments for the millions affected by these diseases.
New medicine prevented disease in mice
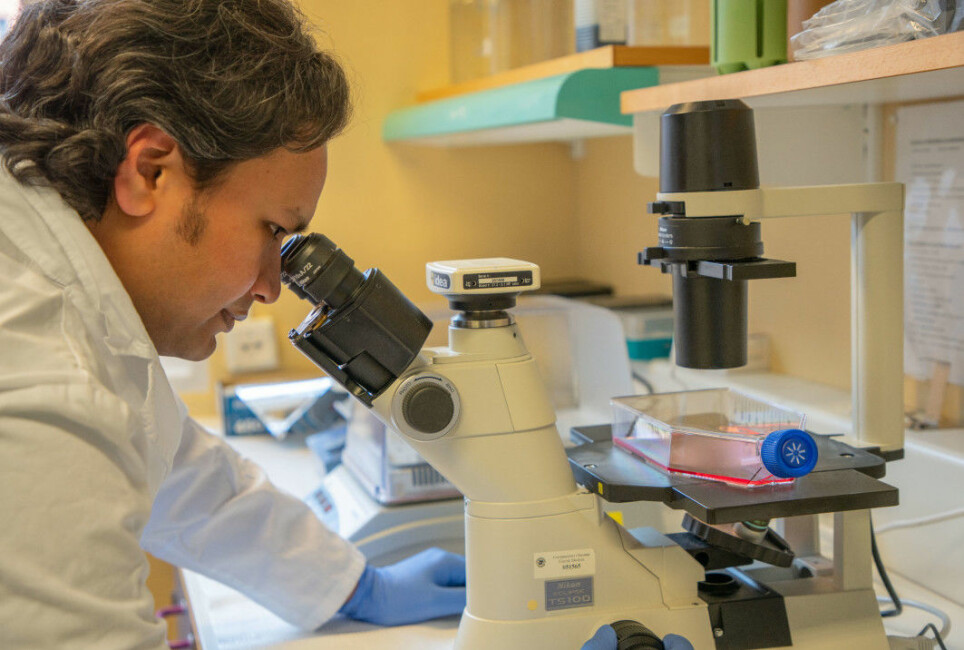
This is where Ashraful Islam from UiT Norway's Arctic University and his international colleagues come in.
They have developed a new type of medicine that influences mechanisms deep in the immune system.
The research team has now tested the medicine on various mice that have been bred to have a high risk of developing a disease similar to three autoimmune diseases: type 1 diabetes, arthritis and autoimmune encephalitis.
The results showed that a single dose of the drug was enough to give the mice long-term protection against developing disease. The drug could also stop the development of the disease and alleviate the symptoms in mice that had already developed one of the three disorders.
The researchers believe that the method could be important for the treatment of autoimmune diseases in humans as well.
Professor Silke Appel at the University of Bergen studies the immune system and autoimmune diseases. She did not participate in this study, but finds it interesting.
“This is a well-conducted study with exciting results,” she wrote in an e-mail.
Antigen-presenting cells
Previous research into the precise mechanisms behind autoimmune disease first put researchers on the trail of the new medicine.
Studies have shown that so-called antigen-presenting cells play a key role.
These cells form a kind of scout patrol that monitors and analyses the surroundings. They pick up interesting things they find as they go, like viruses, bacteria and substances from our food or our environment. They can also gather up parts from the body's own cells.
The antigen-presenting cells break down and process what they detect. And then they do what the name implies: they present pieces of what they have found. The cells simply display these pieces on their surface.
These pieces of foreign substances are called antigens. And if the pieces originate from the body itself, they are called self-antigens.
Can cause tolerance or immune reaction
The display of the antigen-presenting cells does not go unnoticed.
Another important part of the immune system – the T cells – notices the antigens on display. From here, two completely opposite things can happen, depending on the environment around the cells.
If the environment is peaceful – without inflammatory conditions – the T cells interpret the antigens as harmless. In this way, they help in developing tolerance to precisely these antigens.
This is a very important process. In this way, the immune system learns that it doesn’t have to react to harmless substances from our food or our environment.
However, if inflammation is already present in the environment – that is, if parts of the immune system are already on alert – the T cells interpret the antigens as something dangerous. This triggers a very specific process:
The T cells ensure that antibodies are created to combat these very antigens.
Antibodies find and neutralize antigens
An antibody is a small molecule that recognizes a specific antigen – that is, a particular foreign substance. When the antibody finds the antigen, it attaches itself to it. This may be enough to neutralize the foreign substance, or it can help other immune cells find and destroy the foreign substance.
In this way, the antibodies help the body to cope with dangers, like viruses, bacteria and toxins.
But what about when the antigen-presenting cells display self-antigens – substances from our own body?
If this happens with inflammation present in the environment, the immune system may begin to produce antibodies against these self-antigens. These antibodies recognize and bind to the body's own cells and the immune system attacks and destroys them.
This is what causes autoimmune disease. The autoimmune disease in question depends on which cells the T cells react to and which antibodies were made.
In diabetes 1, for example, antibodies are created against the insulin-producing cells in the pancreas.

Possibilities to develop tolerance
This basic knowledge about autoimmune disease tells us how immune responses to our own cells occur. But it also tells us how the body develops tolerance to substances and opens up the possibility of reversing autoimmune disease.
The process uses the body's own system to develop tolerance for exactly those parts of the body that the immune system has previously perceived as dangerous.
If we can get antigen-presenting cells to display self-antigens from the body's own cells in a peaceful situation without inflammatory conditions, we can help the body begin to tolerate them.
Take a person with type 1 diabetes, for example. Have the antigen-presenting cells display pieces of insulin-producing cells under calm conditions. This should in theory teach the T cells that the insulin cells aren’t dangerous after all, so the immune system can stop attacking them.
But how do we accomplish that recognition? And if we do, will it work in practice?
Developed a nanobody
Islam and his colleagues have developed just such a method.
The researchers created a tiny molecule – a nanobody – that recognizes and attaches to the antigen-presenting cells. To this nanobody the researchers connect a self-antigen, or pieces of the body's own cells, that the immune system of a person with autoimmune disease reacts to.
In this way, the researchers can transport self-antigens directly to the antigen-presenting cells – and also ensure that the antigen-presenting cells receive the self-antigens under peaceful conditions with no inflammation.
“This way, we train the cells to develop tolerance,” Islam explains in an e-mail.
Together with colleagues from the USA and Uruguay, he has now tested the nanobody on three different autoimmune diseases in animals. These are similar to type 1 diabetes, arthritis and autoimmune encephalitis.

Prevented autoimmune disease
The medicine worked as the theory suggested: It prevented the disease from developing, and could in some cases also stop the development of mice that were already ill.
It also showed that a tiny little nanobody was a good solution. Such small molecules easily penetrated various tissues in the body, making it easier to get the drug to antigen-presenting cells in different places.
Residues of the nanobodies that weren’t used up also quickly disappeared from the body. This reduces the risk of side effects.
However, Islam stresses that it was important to make sure that no inflammation was present while the treatment was going on.
One way of ensuring non-inflammatory conditions is by giving anti-inflammatory drugs at the same time as the treatment.
Human testing is conceivable
Now, of course, the big question is: Can the technique also be used by humans?
So far, the method has only been tested on relatively small groups of mice, and only on females, says Appel.
In addition, the study showed that different individuals could react quite differently to the treatment. Initially, more research on animals is probably needed to find out more about how the medicine works in the body. But the next step may also become possible.
“It’s quite conceivable that we’ll be able to test this in humans,” says Appel.
In that case, it will be critical to combine the treatment with substances that reduce inflammation, she points out. Because if the antigen-presenting cells pick up the self-antigen in inflammatory conditions, the patient risks the opposite result.
“Instead of tolerance, you would then get an immune response to the antigen and worsen the situation,” Appel says.
This happened in the mouse experiment when the researchers tried to treat mice that had already developed autoimmune disease and had active inflammation in the body.
Could take a long time
One challenge is precisely that the method was most effective in preventing the onset of autoimmune disease in mice, according to Appel.
This is an appropriate form of treatment in an experiment with animals that rapidly develop disease. In humans, however, autoimmune disease can simmer for decades before a person discovers the first symptoms.
In this situation, a person should have received the treatment long before the disease was diagnosed. But so far we have no tests that easily identify people with incipient autoimmune disease.
“This is an incredibly complex system,” says Appel.
“Realistically, it will probably take a while before this can be used to treat people.”
Reference:
Novalia Pishesha et.al.: Induction of antigen-specific tolerance by nanobody–antigen adducts that target class-II major histocompatibility complexes, Nature Biomedical Engineering, June 2021. Abstract.
———































