Dangerous use of antibiotics rises
The use of broad-spectrum antibiotics at Norwegian hospitals rose by 20 percent from 2006 to 2011.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
Norway has had more fortune and success than many other countries in keeping multi-resistant microbes at bay.
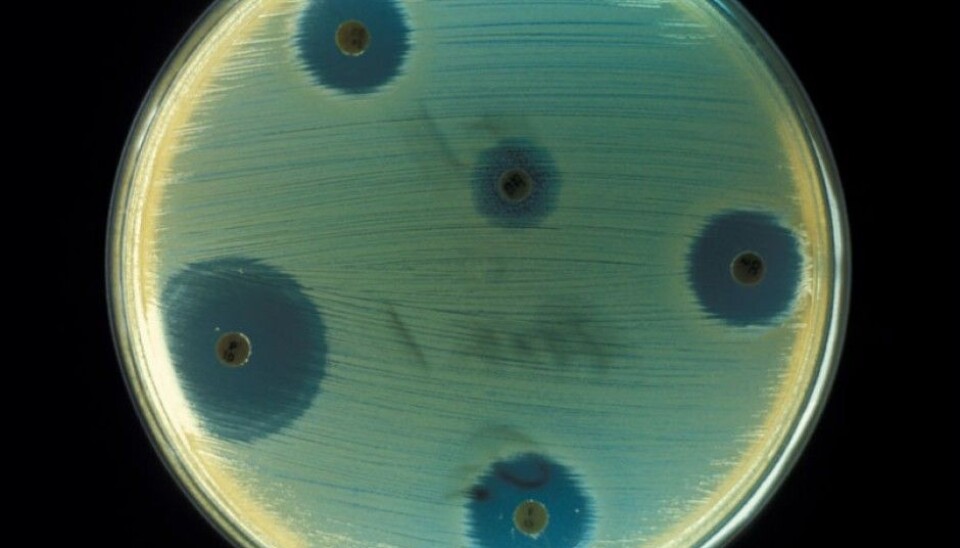
But a new study shows an upsurge in the use of broad-spectrum antibiotics at Norwegian hospitals. This raises the risk of development of microbes that are resistant and unmanageable. In turn this can make it exceedingly difficult to treat even innocuous infectious diseases, let alone the tougher ones.
“This is worrisome. Norwegian hospitals have previously cultivated a conservative culture and been reluctant to use broad-spectrum antibiotics preventively. The study shows a tendency toward jeopardizing this culture, although the use has levelled off the last couple of years nationwide,” says doctor and researcher Jon Birger Haug.
He recently defended his doctoral thesis on his findings at the University of Oslo’s Institute of Clinical Medicine.
A 50 percent rise
Haug found that the use of broad-spectrum antibiotics has increased in two periods at Norwegian hospitals.
At the hospitals run by Norway’s East Regional Health Authority — which includes the greater Oslo area — the use of broad-spectrum antibiotics jumped by 50 percent in the five-year period of 2002- 2007.
The use of broad-spectrum antibiotics, which add to the risk of microbes evolving a dangerous resistance to drugs, rose by 20 percent from 2006 to 2011 nationwide. The use of antibiotics in general rose 17 percent in both periods.
Haug thinks the country needs to buckle down and impose national guidelines for the use of broad-spectrum antibiotics.
“Something has to be done before it’s too late. We still have the chance to avoid getting in the same mess as the rest of the world,” says Haug, who works at Østfold Hospital. He fears we could be facing a post-antibiotics era without this vital medical weapon.
Just to make sure
Why have Norwegian hospitals been using broad-spectrum antibiotics more than before?
“There are several reasons why the usage has increased. Typically, patients who are admitted with even moderate infections are given antibiotics that cover as many types of bacteria as possible. This is done while waiting to see the results of a bacterial culture test, to identify the culprit. Such tests can take as long as three days,” explains Haug.
The medical researcher says one solution is to get faster answers to these tests, which new methods will ensure in the near future.
Advanced methods require antibiotics
On the bright side hospitals are capable of treating more groups of patients than they used to. But this is also one of the reasons for a rise in use of antibiotics.
“We save more lives now in hospitals with the help of new methods of treatment, much because we can initiate post-treatment schemes using antibiotics. But such practice is a double-bladed sword because of its long-term impact on antibiotics,” says Haug.
Greater amounts of antibiotics are needed as more organ transplants are carried out. Such surgery entails the blocking of the immune system with medications to prevent the body from rejecting the new organ.
“The availability of effective antibiotics these cases is a prerequisite for carrying out these life-saving transplants,” he explains.
Cancer patients are also receiving more life-prolonging treatment than they used to get. Such treatment often degrades the normal functions of the immune system. These patients are then susceptible to infections and have a greater need of antibiotics.
There are also geriatric patients who often have weaker immune systems and run higher risks of infections, but their numbers have been relatively stable.
The surprising fact is that much of the increase in use broad-spectrum antibiotics cannot be explained by a rise in patients who need them.
Doctors from other cultures
Haug thinks part of the explanation could be that Norwegian hospitals have expanded their staffs doctors from abroad.
He explains that many of these physicians come from cultures with other traditions, including less restrictions on the use of antibiotics as preventive remedies.
“We used to organise systematic, mandatory courses for doctors from abroad to inform them of our restrictive approach toward the use of antibiotics. We explained the conservative Norwegian attitudes and precautions regarding the use of the most advanced types of antibiotics. These courses are no longer held, apparently because of EU regulations,” says Haug.
Sweden as a model
A whopping 85 percent of the total use of antibiotics is prescribed by doctors outside of Norwegian hospitals. But Haug’s immediate wish is for the country to instigate a better regime for supervising the quantities of antibiotics used in the hospitals.
“National surveillance of the use of antibiotics is imperative if we hope to avoid resistance problems. They have come much further in countries such as Sweden and the Netherlands in this respect. We should look to these countries as our models,” says Haug.
He also urges individual patients — you and me — to be cautious about letting themselves be treated with antibiotics.
“Wait a while. Remember that if you refrain from being treated for a relatively banal infection, you raise the chances that your grandchild will still have the use of antibiotics for serious problems in the future,” he says.
------------
Read the Norwegian version of this article at forskning.no
Translated by: Glenn Ostling


































