Can blood from young people slow down Alzheimer's?
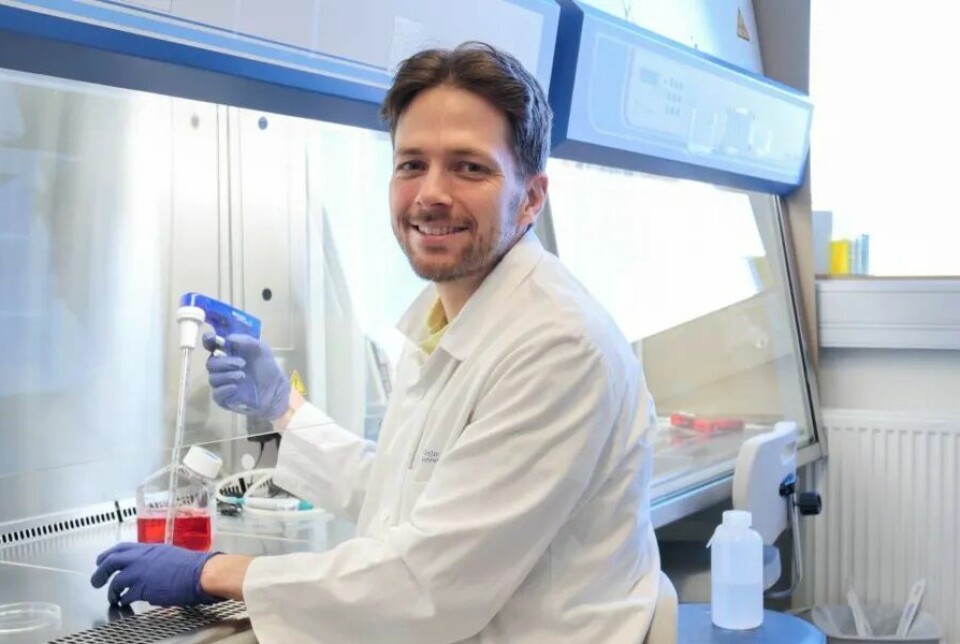
Norwegian researchers are to test a possible new treatment for Alzheimer's disease.
In a new study, patients will have their blood plasma completely replaced with plasma from young donors.
This will be the first time researchers test a total replacement of blood plasma. The study has recently started at Oslo University Hospital (OUS).
Maybe this could become a new treatment against Alzheimer's disease.
The background for the research is special findings made in mice.
Improvements observed in older mice
In somewhat grim experiments, mice have been surgically joined to share circulatory systems. This led to unusual observations.
Older mice connected to younger mice appeared to reap benefits from the latter’s blood, whereas the younger mice seemed to deteriorate when exposed to the older mice’s blood.
The practice of conjoining mice dates back to the 19th century. In 1950, researchers noticed a rejuvenating effect on the older mice’s cartilage when they were paired with younger mice.
This type of research picked up again in the 2000s, according to an article from The New York Times.
Researchers have seen a positive effect in the brains of the old mice and in several types of organs and tissues, according to a research article in Nature Aging. Not all studies are conclusive.
“It suggests that something within the blood or blood cells plays a role in the ageing process,” says Petter Holland, a researcher at OUS.
What is it about young blood that seems to slow down ageing? Does the same apply to humans? These are questions Holland and his team aim to answer.
Can it be used against Alzheimer's disease?
A recently published study has provided researchers with insights into an effect similar to what has been observed in mice.
The study found that transplanted blood cells in humans are influenced by whether they are introduced into an older or younger body. Petter Holland has written about the study in a blog post at Ekspertsykehuset (link in Norwegian).
In this recent study, patients are to receive blood plasma, which is the fluid component of blood and does not include the blood cells.
There have been previous attempts where patients have been given blood plasma from young people or where their own plasma has been diluted. The largest study, called the Ambar study, is from Spain and showed positive results for patients with Alzheimer's disease.
The researchers are now planning to completely replace the blood plasma.
The age of blood cells
Researchers at OUS have looked at how transplanted blood cells are affected by the age of the body they enter.
“We were curious about how ageing processes in cells are affected by the environment,” says Holland.
The researchers used data from bone marrow transplants carried out in Norway and Germany. Many of the transplants were done in connection with treatment for blood cancer.
Bone marrow transplants involve taking stem cells that produce new blood cells from a donor's bone marrow and transferring them to the patient.
The researchers were particularly interested in cases where there was a fairly large age difference between donor and recipient.
The ageing process speeds up
If the stem cells come from a 20-year-old person, the cells’ age is also measured to be 20 years. The cells age by approximately one year each year, Holland explains.
What happens to the young cells when they enter an older body of, for example, 60 years?
The researchers found that the cells began to age faster.
For example, after eight years, the expected age of the cells would be 28 years.
Yet, when introduced into a 60-year-old individual, this ageing process speeds up, possibly resulting in the cells being assessed at an age of 32 years.
“In the case of older cells entering a younger body, we observed the reverse phenomenon. The ageing process within the cells slowed down,” says Holland.
“We believe this provides the first piece of evidence that this phenomenon, previously seen in mice and rats, likely extends to humans too.”
Will replace blood plasma
The new study and other previous research lay the groundwork for the plasma study at OUS.
The study aims to explore if swapping the blood plasma of Alzheimer's patients with that from young donors could slow the progression of the disease.
“The idea is that by influencing or delaying ageing processes, we can also delay the development of age-related diseases,” says Holland. “Dementia stands out as a prime area of focus for us. That's why we're looking into individuals who have just received a dementia diagnosis.”
The blood plasma will be replaced through several rounds over a short period.
This exchange will not only affect the blood's liquid component but also the fluid surrounding the organs, since they are identical.
“The goal is to achieve a complete rejuvenation of the entire fluid environment in the blood and organs,” he says.
Requires many donors
The treatment is done by connecting the patient to a machine that can separate the fluid in the blood from the cells and add new plasma.
Holland assures that this method is safe, based on solid documentation.
"It's a routine procedure in clinical settings to mitigate a variety of conditions, such as removing antibodies during intense autoimmune reactions," he says.
The process is called Therapeutic Plasma Exchange.
How many donors are needed for the patient's blood plasma to be completely replaced in the new study?
Holland does not have an exact number but says that a considerable number of donors per patient is required.
“It’s a treatment that requires a lot from donors,” he says.
Whether the burden is worth it depends on how strong the effect of the treatment is.
“We envision that the final treatment will not depend on donors. We aim to do analyses to find out exactly which molecules might have a beneficial effect and develop a treatment based on that,” he says.
If the pilot study is successful, the plan is to start a larger study.
Researchers are currently recruiting patients. They are also seeking donors, healthy men between the ages of 18 and 25, who can give blood plasma. The hope is that women will also be able to join as donors.
Few participants
Lars Nilsson is professor of pharmacology at the University of Oslo’s Institute of Clinical Medicine and researches Alzheimer's disease.
He notes that the pilot study being starting at Oslo University Hospital is relatively small and aims to include 10 patients. He also refers to a similar study at NTNU, named ExPlas, which has 60 participants.
The ExPlas study involves administering blood plasma from physically fit individuals to patients with Alzheimer's disease.
“With so few patients, it’s unlikely that scientific proof of the treatment’s effectiveness – meaning a statistically significant effect – can be found,” Nilsson believes.
Lack of understanding about the effect
When there are few patients involved, one should have a good understanding of how the treatment is intended to affect the disease’s biology, says Nilsson. Additionally, there should be biomarkers, something to measure, that can reflect a biological effect in the patients' brains.
Nilsson points out a fundamental flaw in studies focused on adding or replacing blood plasma in Alzheimer's patients:
“There’s a lack of understanding of how the treatment affects the disease in the brain at a molecular level. The research started with animal experiments showing that plasma from young animals can positively affect the brains of older animals. From there, it has relatively quickly moved from old mice to patients with Alzheimer’s disease,” he says.
“A clinical study then becomes somewhat of a gamble.”

Even if they were to find a slight trend towards improvement in certain cognitive measures in the patients, it would be difficult to secure funding for a larger patient study when the effect is not statistically significant, Nilsson believes.
“It’s necessary for the treatment to be put into clinical use,” he says.
Something being statistically significant means that it is unlikely that the result is due to chance, luck, or biases in the sample.
Planning a larger study
Petter Holland agrees that the pilot study they plan to conduct initially cannot determine the effect of the treatment. This study must be carried out to demonstrate that it is safe to expose patients to this.
“If the pilot study shows that we can perform the procedures with low risk, we hope to get approval to conduct a larger, randomised study. Exactly how many patients will be included in the randomised study is not yet known. We are actively seeking funding to include as many patients as possible,” he says.
“We will only conduct a randomised study if our power calculations indicate that we have enough participants to determine if the treatment is effective,” he says.
In other words, the researchers will calculate in advance how many patients are needed to obtain a reliable answer about the effect.
———
Illustration at the top of the article: Olga Nikonova / Shutterstock / NTB, edited by sciencenorway.no
Translated by Alette Bjordal Gjellesvik
Read the Norwegian version of this article on forskning.no
Reference:
Holland et al. Epigenetic aging of human blood cells is influenced by the age of the host body. Aging Cell, 2024.