An article from University of Oslo
Cells with a licence to kill
The body's natural killer cells are programmed to kill without the intervention of any safety mechanism. Now researchers know why.
Denne artikkelen er over ti år gammel og kan inneholde utdatert informasjon.
When a virus penetrates the body, the body's own defence system loads its weapons and fires – to kill. But what actually happens when the virus is attacked?
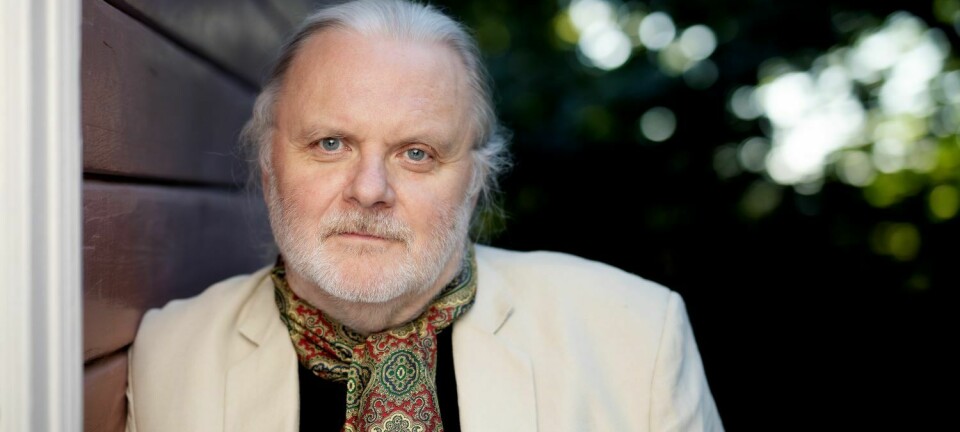
Professor Erik Dissen and research fellow Per Christian Sæther at the Institute of Basic Medical Sciences have done research on the mechanisms employed by the body's natural killer cell, the NK cell, to detect and kill virus-infected cells.
Using mice and rats as models, they have discovered something highly unexpected.
A receptor called CD94/NKG2, which plays a significant role in immune regulation, turns out to be completely different in mice and rats from what researchers had previously assumed, based on studies of human beings.
Our natural defence force
NK cells and T cells are part of our natural immune system and have the task of defending our body from viruses, but T cells need a whole week to develop an immune reaction when a new virus has penetrated the body.
So as not to allow the virus too much free play during that time, other parts of the immune system must step into the breach, because the virus needs to be fought.
Viruses are like small envelopes containing genetic materials that penetrate the cell and take over its synthesising machinery in order to make many new copies of the virus.
"They use our cells as factories to multiply themselves. To take out a virus, you should bomb the whole factory," says Dissen.
In other words, the whole cell has to be eliminated, and that’s what the body's killer cells are there to do.
The NK cells react fast. In a matter of minutes or hours after the virus gains entry, they are ready to attack. The NK cells have two tasks to perform: identify and eliminate.
Now we know what happens, but not how it happens.
The challenge has been to clarify the mechanisms that the NK cells employ to detect virus-infected cells and to determine which molecules are in contact with each other during this process.
Why does the NK cell attack so rapidly, whereas the T cell needs a week to get an immune defence force up and running? Part of the answer may be found in the CD94/NKG2 receptor.
The answer to the mystery
The receptor is expressed on the surface of the NK cell and connects to adaptor proteins, which in turn send a signal that activates the cell's killing machinery.
T cells can divide and become extremely populous. If they attack normal cells, this process of activation is difficult to reverse. Consequently, the T cells have a number of safety mechanisms.
"One of these is that the T cell has two signal paths, both of which must give a go-ahead signal before the T cell is activated and attacks. The NK cell on the other hand has coupled these two signal paths together into a single receptor," explains Dissen.
Adaptor proteins are necessary in order to activate the cell's signal to kill. CD94/NKG2 can connect to two different adaptor proteins simultaneously, both DAP 12 and DAP10.
The former of these represents signal 1, and the latter signal 2. That is why the NK cell can be so quick on the trigger. It does not have the same safety mechanism as the T cells. Instead it has been given a full licence to kill.
The researchers say that this discovery agrees well with what they knew from before - that the NK cell acts quickly. Now they have found out more about why.
Clinical importance?
Will this discovery be of any importance to you and me? If we look and think ahead and begin to speculate, we can imagine areas where this discovery may be important.
Since we are talking about the field of immunology, it is not surprising that autoimmune disorders are mentioned when Dissen starts talking about possible clinical methods of treatment.
He points out that if NK cells play a role in autoimmune disorders, it may be the case that medicines that affect these two molecules can affect the immune response, but they need to learn more about the underlying mechanisms.
The receptors are important in the regulation of the immune response and can thus be possible drug targets, i.e. potential targets for medicines that can have an effect on autoimmune disorders.
"Understanding the signal mechanisms will be a starting point for developing new medicines," says Dissen.
The researchers now know that CD94/NKG2 has both a trigger and a safety mechanism in the same switch. Another small piece of the puzzle has thus been put in place.
Translated by: 09-03-2012 08:00